Association between fasting blood glucose and thyroid stimulating hormones and suicidal tendency and disease severity in patients with major depressive disorder
DOI:
https://doi.org/10.17305/bjbms.2021.6754Keywords:
First-episode drug naïve, major depressive disorder, depression, thyroid hormones, blood glucose, diabetes mellitus, dyslipidemia, hypertension, suicidal behavior, suicidal attemptsAbstract
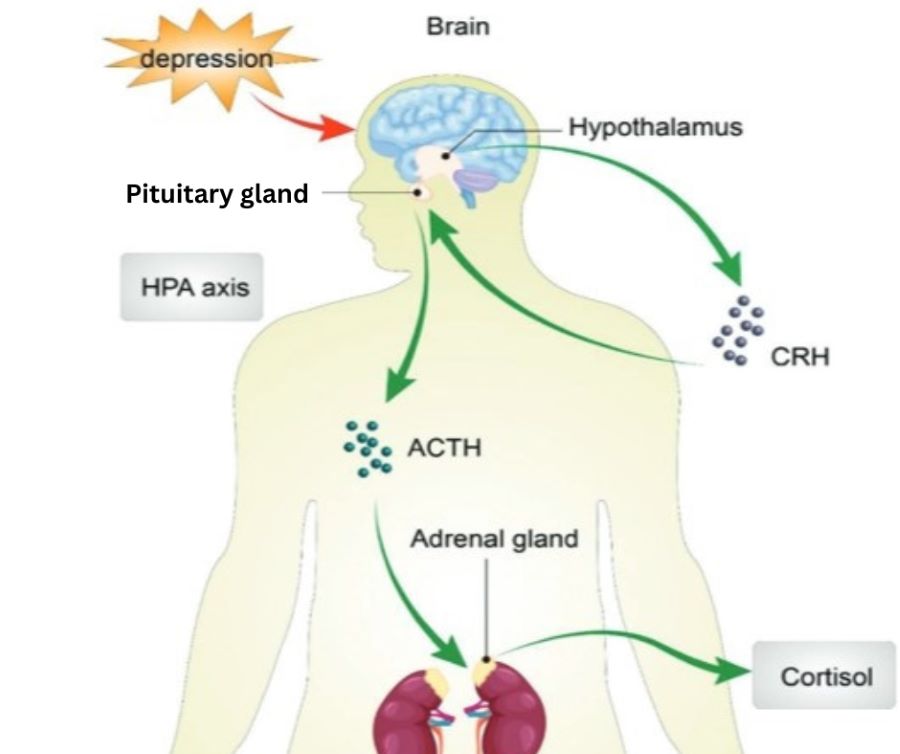
Thyroid dysfunction and diabetes are reported to be associated with depression. However, their role in the suicide risk in patients with major depressive disorder (MDD) is unclear. The purpose of this study was to investigate and compare thyroid dysfunction and diabetes between suicide attempters and non-suicide attempters in a large sample of first-episode drug-naïve (FEND) MDD patients. A descriptive study was conducted on 1279 Chinese outpatients with a diagnosis of first-episode MDD. Their sociodemographic information, blood levels of thyroid hormones, glucose, lipids and body mass index (BMI) parameters were collected. The positive subscales of the positive and negative syndrome scale (PANSS), Hamilton Anxiety Rating Scale (HAMA), Hamilton Depression Rating Scale (HAMD) were measured for psychotic, anxiety and depressive symptoms. Our results showed that compared with non-suicide attempters (P<0.01), suicide attempters had statistically higher scores on HAMD, HAMA and PANSS psychotic symptoms, as well as higher thyroid stimulating hormone (TSH) serum levels, glucose, anti-thyroglobulin (A-TG), anti-thyroid peroxidase (A-TPO), total cholesterol (TC), triglycerides (TG), low density lipoprotein cholesterol (LDL-C), systolic blood pressure and diastolic blood pressure (all with P<0.001). These results revealed that TSH, A-TG, A-TPO, TC, TG and LDL-C may be promising biomarkers of suicide risk in MDD, implying the importance of regular assessment of blood glucose level and thyroid function parameters for suicide prevention, along with possible treatment for impaired thyroid function and diabetes for the suicide intervention in MDD patients. Such patients with abnormal blood sugar and TSH must undergo thorough screening for suicidal ideation.
Citations
Downloads
Downloads
Additional Files
Published
License
Copyright (c) 2022 Weiting Liu, Zezhen Wu, Min Sun, Shuo Zhang, Juan Yuan, Dan Zhu, Guimimg Yan, Kaijian Hou

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-02-17
Published 2022-07-29









