Thiersch graft follow-up with narrow band imaging for acquired atresia of the external auditory canal: Canaloplasty with Thiersch graft versus vascularization evaluated with narrow band imaging
DOI:
https://doi.org/10.17305/bjbms.2021.6876Keywords:
Acquired atresia, narrow-band imaging, withe light, Thiersch graftAbstract
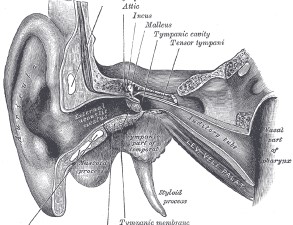
Acquired atresia of the external ear canal is a narrowing of the external ear canal (EAC) that appears obstructed by fibrous tissue or bone tissue. Acquired atresia has two different phases: wet and dry stage. Computed tomography (CT) scan may show a scan where soft tissue fills EAC. Treatment may be medical and/or surgical. The surgical treatment of choice is represented by canaloplasty with a skin-free flap. To our knowledge, no article has reported data on the analysis of vascularization of acquired atresia of the external ear canal and vascularization of skin flap during follow-up with narrow-band imaging. This study evaluated patients suffering from acquired atresia of the external auditory duct, treated surgically in our Department of Organi di Senso of Sapienza University, from 2017 to 2020. All patients underwent: anamnestic collection, physical examination, CT. Preoperative and postoperative otoendoscopic evaluation (1,3,6 and12 months) was performed with both cold white light endoscopic vision (CWL) and narrowband imaging (NBI). 17 patients were enrolled in the study. Preoperative otoendoscopic examination of WL showed stenosis with a diameter <75% and a tympanic membrane not viewable in all patients. At 12 months of follow-up, 94% of patients had no recurrence of external ear canal stenosis. 88% of patients had normal NBI light vascularization. Our study evaluated how NBI can be a superior method, compared to CWL, to assess the state of the flap and can be relevant in the decision-making process of a re-intervention.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2022 Annalisa Pace, Valeria Rossetti, Irene Claudia Visconti, Alessandro Milani, Giannicola Iannella, Antonino Maniaci, Salvatore Cocuzza, Giuseppe Magliulo

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-02-08
Published 2022-09-16









