LGALS3 and AXIN1 gene variants playing role in the Wnt/ β-catenin signaling pathway are associated with mucinous component and tumor size in colorectal cancer
DOI:
https://doi.org/10.17305/bjbms.2016.721Keywords:
Colorectal Cancer, LGALS3, AXIN1, ASO-PCR, PCR-RFLPAbstract
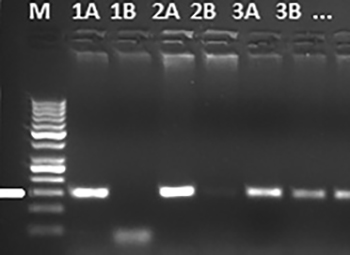
The Wnt pathway alterations have been identified in colorectal and many other cancer types. It has been reported that galectin-3 (which is encoded by the LGALS3 gene) alters the signaling mechanism in the Wnt/ β-catenin pathway by binding to β-catenin in colon and other cancers. AXIN1 is mainly responsible for the assembly of the β-catenin destruction complex in the Wnt pathway. This study investigated the relationship of rs4644 and rs4652 variants of the LGALS3 gene and rs214250 variants of the AXIN1 gene to histopathological and clinical properties. Our study included a total of 236 patients, of whom 119 had colorectal cancer (42 women, 77 men) and 117 were healthy controls. Polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP) and allele-specific oligonucleotide (ASO) PCR methods were used. In addition, the serum galectin-3 level was studied with the enzyme-linked immunosorbent assay (ELISA) method. For the rs4644 variant of the LGALS3 gene, the CC genotype a mucinous component was significantly more common than those without a mucinous component (p=0.026). C allele frequency of the rs214250 variant of the AXIN1 gene was significantly correlated to tumor size in the advanced tumor stage (p=0.022). The CCAACT haplotype was more common in colorectal cancer patients (p=0.022). Serum galectin-3 level was higher in the patient group compared to the control group (5.9± 0.69 ng/ml vs. 0.79±0.01 ng/ml; p<0.001). In conclusion, variants of LGALS3 and AXIN1 genes affect tumor sizes and the mucinous component via Wnt/ β-catenin pathway in the pathogenesis of colorectal cancer.
Citations
Downloads
References
Boyle P, Elena M. Epidemiology of colorectal cancer. British Med Bull. 2002;64:1–25.
http://dx.doi.org/10.1093/bmb/64.1.1
Bernard W, Stewart P, Christopher PW. World Cancer Report. Retrieved 24 May 2007.
Paula MC, Harold F. The genetics of CRC. Ann Intern Med. 2002 Oct 1;137(7):603-12.
Rasool S, Ganai BA, Sameer AS, Masood A. Esophageal cancer: associated factors with special reference to the Kashmir Valley. Tumori. 2012 Mar-Apr;98(2):191-203.
Colussi D, Brandi G, Bazzoli F, Ricciardiello L. Molecular pathways involved in colorectal cancer: implications for disease behavior and prevention. Int J Mol Sci. 2013 Aug 7;14(8):16365-85.
http://dx.doi.org/10.3390/ijms140816365
Di Lella S, Sundblad V, Cerliani JP, Guardia CM, Estrin DA, Vasta GR, et al. When galectins recognize glycans: from biochemistry to physiology and back again. Biochemistry. 2011 Sep 20;50(37):7842-57.
http://dx.doi.org/10.1021/bi201121m
Newlaczyl A, YuL G. Galectin-3 a jack of all trades in cancer. Cancer Lett. 2011 Dec 27;313(2):123-8.
http://dx.doi.org/10.1016/j.canlet.2011.09.003
Yu F, Finley RL Jr, Raz A, Kim HR. Galectin-3 translocates to the perinuclear membranes and inhibits cytochrome c release from the mitochondria. A role for synexin in galectin-3 translocation. J Biol Chem. 2002 May 3;277(18):15819-27.
http://dx.doi.org/10.1074/jbc.M200154200
Song S, Mazurek N, Liu C, Sun Y, Ding QQ, Liu K,et al. Galectin-3 mediates nuclear beta-catenin accumulation and Wnt signaling in human colon cancer cells by regulation of glycogen synthase kinase-3beta activity. Cancer Res. 2009 Feb 15;69(4):1343-9.
http://dx.doi.org/10.1158/0008-5472.CAN-08-4153
Shimura T1, Takenaka Y, Tsutsumi S, Hogan V, Kikuchi A, Raz A. Galectin-3, a novel binding partner of β-catenin. Cancer Res. 2004 Sep 15;64(18):6363-7.
http://dx.doi.org/10.1158/0008-5472.CAN-04-1816
Iacovazzi PA1, Notarnicola M, Caruso MG, Guerra V, Frisullo S, Altomare DF, et al. Serum levels of galectin-3 and its ligand 90k/mac-2bp in colorectal cancer patients. Immunopharmacol Immunotoxicol. 2010 Mar;32(1):160-4.
http://dx.doi.org/10.3109/08923970902936880
Zaia Povegliano L, Oshima CT, de Oliveira Lima F, Andrade Scherholz PL, Manoukian Forones N. Immunoexpression of galectin-3 in colorectal cancer and its relationship with survival. J Gastrointest Cancer. 2011 Dec;42(4):217-21.
http://dx.doi.org/10.1007/s12029-010-9189-1
Mazurek N, Byrd JC, Sun Y, Hafley M, Ramirez K, Burks J, Bresalier RS. Cell-surface galectin-3 confers resistance to TRAIL by impeding trafficking of death receptors in metastatic colon adenocarcinoma cells. Cell Death Differ. 2012 Mar;19(3):523-33.
http://dx.doi.org/10.1038/cdd.2011.123
Hill M, Mazal D, Biron VA, Pereira L, Ubillos L, Berriel E, et al. A novel clinically relevant animal model for studying galectin-3 and its ligands during colon carcinogenesis. J Histochem Cytochem. 2010 Jun;58(6):553-65.
http://dx.doi.org/10.1369/jhc.2010.955237
Mahmoud LK, Arfaoui A, Khiari M, Chaar I, El Amine O, Hmida AM, et al. Loss of galectin-3 expression in mucinous colorectal carcinomas is associated with 5'CpG island methylation in Tunisian patients. Appl Immunohistochem Mol Morphol. 2011 May;19(3):258-65.
Greco C, Vona R, Cosimelli M, Matarrese P, Straface E, Scordati P, et al. Cell surface overexpression of galectin-3 and the presence of its ligand 90k in the blood plasma as determinants in colon neoplastic lesions. Glycobiology. 2004 Sep;14(9):783-92.
http://dx.doi.org/10.1093/glycob/cwh092
N. Cancer Genome Atlas. Comprehensive molecular characterization of human colon and rectal cancer, Nature. 2012; 487:330–337.
http://dx.doi.org/10.1038/nature11252
Altshuler DM, Durbin RM, Abecasis GR, Bentley DR, Chakravarti A, Clark AG, et al. An integrated map of genetic variation from 1,092 human genomes, Nature 2012 Nov 1;491(7422):56-65.
http://dx.doi.org/10.1038/nature11632
Mazzoni SM, Fearon ER. AXIN1 and AXIN2 variants in gastrointestinal cancers. Cancer Lett. 2014 Dec 1;355(1):1-8.
http://dx.doi.org/10.1016/j.canlet.2014.09.018
Shimizu Y, Ikeda S, Fujimori M, Kodama S, Nakahara M, Okajima M, et al. Frequent alterations in the Wnt signaling pathway in colorectal cancer with microsatellite instability. Genes Chromosomes Cancer. 2002 Jan;33(1):73-81.
http://dx.doi.org/10.1002/gcc.1226
Serman L, Martic NT, Serman A, Vranic S. Epigenetic alterations of the Wnt signaling pathway in cancer: a mini review. Bosn J Basic Med Sci. 2014 November; 14(4): 191–194.
http://dx.doi.org/10.17305/bjbms.2014.4.205
Khan NP1, Pandith AA, Hussain MU, Yousuf A, Khan MS, Wani KA, et al. Novelty of Axin 2 and lack of Axin 1 gene mutation in colorectal cancer: a study in Kashmiri population. Mol Cell Biochem. 2011 Sep;355(1-2):149-55.
http://dx.doi.org/10.1007/s11010-011-0848-8
Jin LH1, Shao QJ, Luo W, Ye ZY, Li Q, Lin SC. Detection of point mutations of the Axin1 gene in colorectal cancers. Int J Cancer. 2003 Dec 10;107(5):696-9.
http://dx.doi.org/10.1002/ijc.11435
Sue Ng S, Mahmoudi T, Li VS, Hatzis P, Boersema PJ, Mohammed S, et al. MAP3K1 functionally interacts with Axin1 in the canonical Wnt signalling pathway. Biol Chem. 2010 Feb-Mar;391(2-3):171-80.
http://dx.doi.org/10.1515/bc.2010.028
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011 Mar-Apr;61(2):69-90.
http://dx.doi.org/10.3322/caac.20107
Prenen H, Vecchione L, Van Cutsem E. Role of targeted agents in metastatic colorectal cancer. Target Oncol. 2013 Jun;8(2):83-96.
http://dx.doi.org/10.1007/s11523-013-0281-x
Anastas JN, Moon RT. WNT signalling pathways as therapeutic targets in cancer. Nat. Rev. Cancer 2013 Jan;13(1):11-26.
http://dx.doi.org/10.1038/nrc3419
Papkoff J, Rubinfeld B, Schryver B, Polakis P. Wnt-1 regulates free pools of catenins and stabilizes APC-catenin complexes. Mol Cell Biol. 1996 May;16(5):2128-34.
http://dx.doi.org/10.1128/MCB.16.5.2128
Zhang D, Chen ZG, Liu SH, Dong ZQ, Dalin M, Bao SS, et al. Galectin-3 gene silencing inhibits migration and invasion of human tongue cancer cells in vitro via downregulating β-catenin. Acta Pharmacol Sin. 2013 Jan;34(1):176-84.
http://dx.doi.org/10.1038/aps.2012.150
Wang LP, Chen SW, Zhuang SM, Li H, Song M. Galectin-3 accelerates the progression of oral tongue squamous cell carcinoma via a Wnt/β-catenin-dependent pathway. Pathol Oncol Res. 2013 Jul;19(3):461-74.
http://dx.doi.org/10.1007/s12253-013-9603-7
Wang M1, Zhang YC, Yang XY, Wang ZQ. Prognostic significance of the mucin component in stage III rectal carcinoma patients. Asian Pac J Cancer Prev. 2014;15(19):8101-5.
http://dx.doi.org/10.7314/APJCP.2014.15.19.8101
Le Lee DW, Han SW, Lee HJ, Rhee YY, Bae JM, Cho NY, et al. Prognostic implication of mucinous histology in colorectal cancer patients treated with adjuvant FOLFOX chemotherapy. Br J Cancer. 2013 May 28;108(10):1978-84.
http://dx.doi.org/10.1038/bjc.2013.232
Shiono S, Saito T, Fujii H, Arakawa A, Nakamura T, Yao T. A case of Krukenberg carcinoma metastasized from colon cancer resembling mucinous cystadenocarcinoma of the ovary. Int J Clin Exp Pathol. 2013 Dec 15;7(1):394-401.
Akkiprik M1, Celikel CA, Düşünceli F, Sönmez O, Güllüoğlu BM, Sav A, et al. Relationship between overexpression of ras p21 oncoprotein and K-ras codon 12 and 13 mutations in Turkish colorectal cancer patients. Turk J Gastroenterol. 2008 Mar;19(1):22-7.
Kawasaki T, Ohnishi M, Suemoto Y, Kirkner GJ, Liu Z, Yamamoto H, et al. WRN promoter methylation possibly connects mucinous differentiation, microsatellite instability and CpG island methylator phenotype in colorectal cancer. Mod Pathol. 2008 Feb;21(2):150-8.
http://dx.doi.org/10.1038/modpathol.3800996
Nosho K, Shima K, Irahara N, Kure S, Firestein R, Baba Y, et al. SIRT1 histone deacetylase expression is associated with microsatellite instability and CpG island methylator phenotype in colorectal cancer. Mod Pathol. 2009 Jul;22(7):922-32.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2015-10-18
Published 2016-02-04









