Methylation pattern of caveolin-1 in prostate cancer as potential cfDNA biomarker
DOI:
https://doi.org/10.17305/bjbms.2022.7497Keywords:
prostate cancer, biomarker, cfDNA methylation, CAV1Abstract
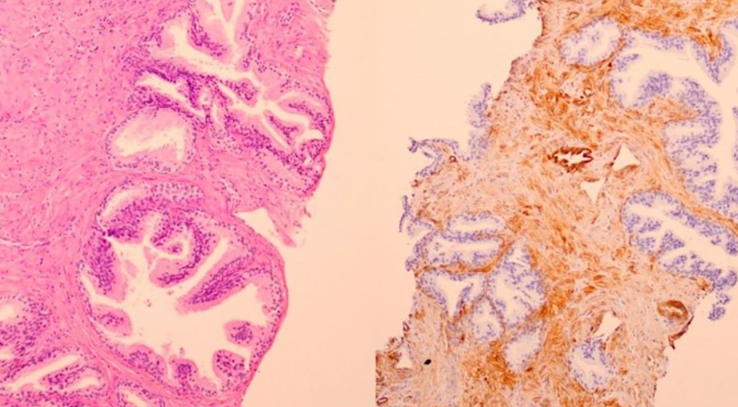
High prevalence and mortality of prostate cancer (PCa) are well known global health issues. Novel biomarkers for better identifying patients with PCa are the subject of extensive research. Prostate specific antigen (PSA) shows low specificity in screening and diagnostics, leading to unnecessary biopsies and health costs. Eighty patients with PCa and benign prostate hyperplasia (BPH) were included in the study. We analyzed CAV1 gene expression and methylation in tissue. CAV1 cfDNA methylation from blood and seminal plasma was accessed as a potential PCa biomarker. Although methylation in blood plasma did not differ between PCa and BPH patients, methylation in seminal plasma showed better PCa biomarker performances than tPSA (AUC 0.63 vs. AUC 0.52). Discrimination of BPH and Gleason grade group 1 PCa patients from patients with higher Gleason grade groups revealed very good performance as well (AUC 0.72). CAV1 methylation is useful biomarker with potential for further seminal plasma cfDNA research, but its diagnostic accuracy should be improved, as well as general knowledge about cfDNA in seminal plasma.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2022 Lucija Škara, Tonći Vodopić, Ivan Pezelj, Irena Abramovic, Borna Vrhovec, Alen Vrtarić, Nino Sincic, Davor Tomas, Stela Bulimbašić, Tomislav Kuliš, Monika Ulamec

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-08-01
Published 2023-01-06









