Analysis of cardiac manifestation and treatment of multisystem inflammatory syndrome in children related to SARS-CoV-2
DOI:
https://doi.org/10.17305/bjbms.2022.7820Keywords:
Acute myocardial dysfunction, shock, pediatric, SARS-CoV-2, MIS-CAbstract
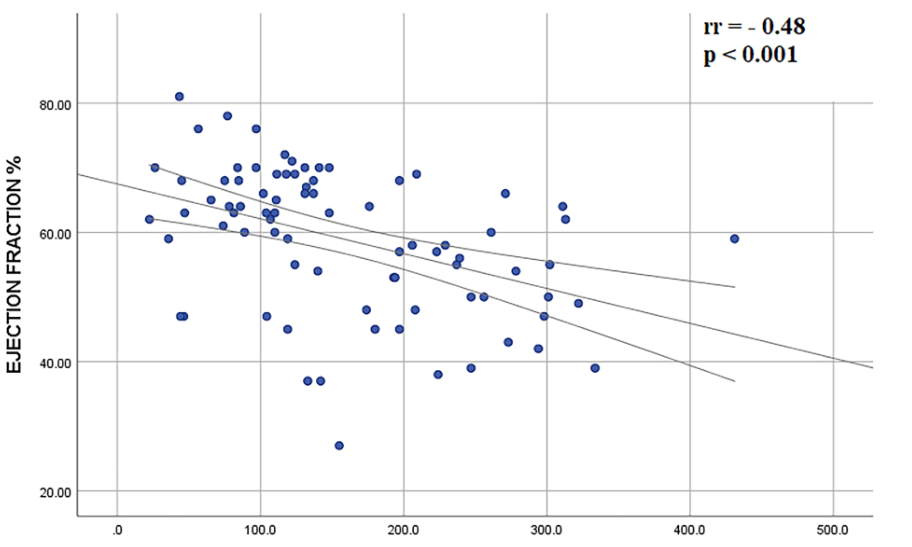
Cardiovascular manifestations are common (35–100%) in the multisystem inflammatory syndrome in children. Our study aimed to analyze treatment impact and cardiovascular involvement in patients with multisystem inflammatory syndrome in children. The retrospective cohort included 81 patients treated between April 2020 and December 2021 (9.3±4.6 years). Elevated cardiac troponin I and pro-B-type natriuretic peptide were observed in 34.2% and 88.5% of patients, respectively. Myocardial dysfunction was observed in 50.6%. Children older than 10 years had a 4-fold increased risk of myocardial dysfunction (odds ratio [OR] 3.6, 95% confidence interval [CI] 1.4-8.9; p=0.006). A moderate negative correlation was proved between left ventricle ejection fraction and C-reactive protein (rr = - 0.48; p < 0.001). More than one-fifth of the patients presented with shock. Coronary artery dilatation was observed in 6.2% of patients. Mild pericardial effusion was detected in 27.1% of children. On standard electrocardiogram, 52.6% of children had negative T waves in the inferior and/or precordial leads; transient QTc prolongation was registered in 43% of patients. Treatment failure was observed in 19 patients. Patients initially treated with intravenous immunoglobulins had 10-fold higher chances for treatment failure than patients treated with corticosteroids (OR 10.6, 95% CI 3,18 – 35.35; p < 0.001). Cardiovascular manifestations were observed in more than half of the patients, with acute myocardial dysfunction being the most common, especially in children older than 10 years. We established a negative association between the degree of elevation of inflammatory markers and left ventricular ejection fraction. Patients treated with intravenous immunoglobulins who had cardiovascular manifestations had treatment failures more frequently than patients treated with corticosteroids.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2022 Stasa Krasic, Sanja Ninic, Sergej Prijic, Sasa Popovic, Srdjan Pasic, Gordana Petrovic, Boris Zec, Snezana Ristic, Dejan Nesic, Luka Nikolic, Vladislav Vukomanovic

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-08-15
Published 2023-03-16









