Brachiomedian artery (arteria brachiomediana) revisited: a comprehensive review
DOI:
https://doi.org/10.17305/bjbms.2016.801Keywords:
Arteria brachiomediana, arteria brachiomediana superficialis, arterial variation, brachiomedian artery, superficial brachiomedian arteryAbstract
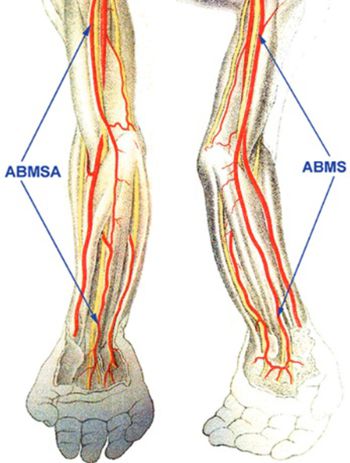
This article reviews in detail the superficial brachiomedian artery (arteria brachiomediana superficialis), a very rare variant of the main arterial trunks of the upper limb. It branches either from the axillary artery or the brachial artery, descends superficially in the arm (similar to the course of the superficial brachial artery) and continues across the cubital fossa, runs superficially in the forearm, approaches the median nerve and enters the carpal canal to reach the hand. It usually terminates in the superficial palmar arch. The first drawing was published, in 1830, and the first description was published, in 1844. Altogether, to our knowledge, only 31 cases of a true, superficial brachiomedian artery have been reported (Some cases are incorrectly reported as superficial brachioradiomedian artery or superficial brachioulnomedian artery). Based on a meta-analysis of known, available studies, the incidence is 0.23% in Caucasians and 1.48% in Mongolians. Knowing whether or not this arterial variant is present is important in clinical medicine and relevant for: The catheterization via the radial or ulnar artery; harvesting the vascular pedicle for a forearm flap based on the radial, ulnar or superficial brachiomedian arteries; the possible collateral circulation in cases of the arterial closure; and the surgical management of carpal tunnel syndrome. Its presence can elevate the danger of an injury to the superficially located variant artery or of an accidental injection.
Citations
Downloads
References
De Garis CF, Swartley WB. The axillary artery in white and Negro stocks. Am J Anat 1928; 41:353-97. http://dx.doi.org/10.1002/aja.1000410208.
Konarik M, Kachlik D, Baca V. A coincidental variation of the axillary artery: the brachioradial artery and the aberrant posterior humeral circumflex artery passing under the tendon of the latissimus dorsi muscle. Bosn J Basic Med Sci 2014; 14(4):239-43. http://dx.doi.org/10.17305/bjbms.2014.4.31.
Lippert H, Pabst R. Arterial Variations in Man, Munich: J.F. Bergmann; 1985. p. 71-3. http://dx.doi.org/10.1007/978-3-642-80508-0_35
http://dx.doi.org/10.1007/978-3-642-80508-0.
Trotter MI, Henderson JL, Gass H, Brua RS, Weisman S, Agress H. The origin of branches of the axillary arteries in white and American Negros. Anat Rec 1930; 46:133-7. http://dx.doi.org/10.1002/ar.1090460205.
Valsecchi O, Vassileva A, Musumeci G, Rossini R, Tespili M, Guagliumi G, et al. Failure of transradial approach during coronary interventions: Anatomic considerations. Catheter Cardiovasc Interv 2006; 67(6):870-8. http://dx.doi.org/10.1002/ccd.20732.
FCAT. Terminologia Anatomica, Stuttgart: Thieme Verlag; 1998.
Bergman RA, Afifi AK, Miyauchi R. Opus II: Cardiovascular System: Arteries: Upper Limb. In: Illustrated Encyclopedia of Human Anatomic Variation; 1992–2004. Available from: http://www.anatomyatlases.org/AnatomicVariants/Cardiovascular/Text/Arteries/Median.shtml [Last accessed on 2016 Mar 8].
Rodríguez-Niedenführ M, Sañudo JR, Vázquez T, Nearn L, Logan B, Parkin I. Median artery revisited. J Anat 1999; 195:57-63.
http://dx.doi.org/10.1046/j.1469-7580.1999.19510057.x, http://dx.doi.org/10.1017/S0021878299005075.
Natsis K, Iordache G, Gigis I, Kyriazidou A, Lazaridis N, Noussios G, et al. Persistent median artery in the carpal tunnel: Anatomy, embryology, clinical significance, and review of the literature. Folia Morphol (Warsz) 2009; 68:193-200.
Singla RK, Kaur N, Dhiraj GS. Prevalence of the persistant median artery. J Clin Diagn Res 2012; 6(9):1454-7.
Rodríguez-Niedenführ M, Vázquez T, Nearn L, Ferreira B, Parkin I, Sañudo JR. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat 2001; 199:547-66.
http://dx.doi.org/10.1046/j.1469-7580.2001.19950547.x.
George BJ, Henneberg M. High frequency of the median artery of the forearm in South African newborns and infants. S Afr Med J 1996; 86(2):175-6.
Henneberg M, George BJ. A further study of the high incidence of the median artery of the forearm in Southern Africa. J Anat 1992; 181:151-4.
Henneberg M, George BJ. High incidence of the median artery of the forearm in a sample of recent southern African cadavers. J Anat 1992; 180:185-8.
Monro A. Outlines of the anatomy of the human body, in its sound and diseases state. Edinburgh: Archibald Constable & Co.; 1813.
Rodríguez-Niedenführ M, Burton GJ, Deu J, Sañudo JR. Development of the arterial pattern in the upper limb of staged human embryos: Normal development and anatomic variations. J Anat 2001; 199:407-17. http://dx.doi.org/10.1046/j.1469-7580.2001.19940407.x.
Green PH. An Account of the Varieties in the Arterial System of the Human Body. Dublin: James Marshal Leckie; 1830. p. 16-20.
Meckel JF. Ueber den regelwidrigen verlauf der armpulsadren [Article in German]. Dtsch Arch Physiol 1816;2:117-31.
Quain R. Anatomy of the arteries of the human body. London: Taylor and Walton; 1844. p. 326-37.
Tiedemann F. Supplementa ad tabulas arteriarum corporis humani (Supplements to tables of Arteries of the human body) [In Latin]. Heidelberg; 1846.
Gruber W. Über die neue und konstante Ellenbogenschlagader des Menschen (Arteria plicae cubiti superficialis) nebst deren Anomalien, der Arteria mediana antibrachii superficialis and ulnaris superficialis. (On new and constant elbow artery (arteria plicae cubiti superficialis) and other anomalies (arteria mediana antibrachii superficialis and ulnaris superficialis)) [In German]. Z Ges Arztezu Wien 1852; 8:481-99.
Gruber W. Über die Arteria mediana antibrachii superficialis, Arteria ulnaris antibrachii superficialis und Duplicität der Arteria ulnaris (On Arteria mediana antibrachii superficialis, arteria ulnaris antibrachii superficialis und duplication of arteria ulnaris) [In German]. Arch Anat Physiol Wissen Med 1867:668-87.
Calori L. Delle anomalie piu importanti di ossa, vasi, nervi e muscoli occorse nell'ultimo biennio facendo anatomia del corpo umano (On important anomalies of bones, vessels, nerves and muscles observed in last two years doing human anatomy) [In Italian]. Mem Acad Sci Bol 1868; 8:417-82.
Parisot L. Consideration’s sur les anomalies de i'artere humerale. Comput Rend Soc Med Nancy 1869; 1:1-28. (in French).
Giacomini C. Prematura divisione dell'arteria del braccio (sotto-varietà mediana). l’osservatore (Observation of premature division of brachial (subvariant of median artery)) [In Italian]. Gaz Clin Torino 1884; 200:129-40.
Testut L. Traité d’Anatomie Humaine [In French]. 3rd ed., Vol. 1. Fascicle 1. Paris: Octave Doin; 1895. p. 1010.
Schwalbe E. Beitrag zur kenntniss der arterienvarietäten des menschlichen armes (Contribution to knowledge of arterial variations of the human arm) [Article in German]. Morphol Arb 1898; 8:1-47.
Müller E. Beiträge zur morphologie des gefässsystems. 1. Die armarterien des menschen. Anat Hefte Abt 1903; 22:379-574. (in German).
Hoskins ER. Persistent arteriae brachii superficialis, antibrachii superficialis et mediana. Anat Rec 1914; 8:421-2.
Dubreuil-Chambardel L. Variations des artères du membre superieur. Paris: Masson et Cie; 1926. p. 180-92. (in French).
Dubreuil-Chambardel L. Variations artérielles rares (Rare arterial variaitons) [In French]. In: Bulletins et Mémoires de la Société D'anthropologie de Paris, VII. Série, tome 8; 1927. p. 86-92. http://dx.doi.org/10.3406/bmsap.1927.9087.
Schwyzer AG, De Garis CF. Three diverse patterns of the arteria brachialis superficialis in man. Anat Rec 1935; 63:405-16. http://dx.doi.org/10.1002/ar.1090630408.
Maruyama K. Seltene varietät der arterien der oberen extremität bei einem Japaner (A. brachialis superficialis lateralis inferior, A. antebrachialis superficialis mediano-ulnaris, arcus volaris superficialis vom typus mediano-ulnaris) (Rare variation of arteries of upper limb observed in a Japanese) [In German]. Folia Anat Jpn 1944; 22:551-67.
http://dx.doi.org/10.2535/ofaj1936.22.6_551.
McCormack LJ, Cauldwell EW, Anson BJ. Brachial and antebrachial arterial patterns: a study of 750 extremities. Surg Gynecol Obstet 1953; 96(1):43-54.
Mrázková O. Ontogenetic development of the median artery in man. Folia Morphol (Praha) 1975; 23(2):170-4.
Nakatani T, Izumi A, Tanaka S. Bilateral superficial median arteries. J Anat 1999;
:475-7. http://dx.doi.org/10.1046/j.1469-7580.1999.19430475.x.
Darwish HH, Khan MM, Zaher WA. Superficial median artery arises from brachioradial artery: a rare variation. Eur J Anat 2008; 12:63-6.
Jelev L, Georgiev GP. A rare case of superficial median artery of high brachial origin: anatomical and clinical considerations of the superficial brachiomedian artery. Anatomy 2010; 5:39-43.
Kachlik D, Hajek P, Konarik M, Krchov M, Baca V, et al. Coincidence of superficial brachiomedian artery and bitendinous palmaris longus: a case report. Surg Radiol Anat 2016; 38(1):147-51. http://dx.doi.org/10.1007/s00276-015-1512-x.
Poynter CW. Congenital anomalies of the arteries and veins of the human body with bibliography, Vol. 22. Lincoln: The University Studies of the University of Nebraska; 1922. p. 1-106.
Lieffring JJ. De quelques variations artérielles à la face antérieure du membre supérieur. (La coïncidence du développement de l'artère du nerf médian avec la naissance prématurée des artères cubitale et radiale) (On several arterial variations of the anterior surface of the upper limb. (The coincidence of development of the median artery and high origin of ulnar and radial arteries)) [In French]. In: Bull Mémoir Soc d'anthropol Paris, VII Série, Tome 5.; 1924. p. 67-77.
Adachi B. Das arteriensystem der Japaner, Kyoto: Maruzen; 1928. p. 285-356. (in German).
Keen JA. A study of the arterial variations in the limbs, with special reference to symmetry of vascular patterns. Am J Anat 1961; 108:245-61.
http://dx.doi.org/10.1002/aja.1001080303.
Lengele B, Dhem A. Unusual variations of the vasculonervous elements of the human axilla. Report of three cases. Arch Anat Histol Embryol 1989; 72:57-67.
Singer E. Embryological pattern persisting in arteries of the arm. Anat Rec 1933; 55:403-9. http://dx.doi.org/10.1002/ar.1090550407.
Rodríguez-Baeza A, Nebot J, Ferreira B, Reina F, Pérez J, Sañudo JR, et al. An anatomical study and ontogenetic explanation of 23 cases with variations in the main pattern of the human brachio-antebrachial arteries. J Anat 1995; 187(2):473-9.
Arey LB. Developmental anatomy. In: Development of the arteries, 6th ed. Philadelphia: W.B. Saunders Co.; 1957. p. 375-7.
Jurjus AR, Correa-De-Aruaujo R, Bohn RC. Bilateral double axillary artery: embryological basis and clinical implications. Clin Anat 1999; 12(2):135-40.
http://dx.doi.org/10.1002/(SICI)1098-2353(1999)12:2<135::AID-CA10>3.0.CO;2-M, http://dx.doi.org/10.1002/(SICI)1098-2353(1999)12:2<135::AID-CA10>3.3.CO;2-D.
Kopuz C, Gülman B, Baris S. Persistent median artery: an anatomical study in neonatal and adult cadavers. Kaibogaku Zasshi 1995; 70(6):577-80.
Jaschtschinski SN. Morphologie und topographie des Arcus volaris sublimis und profundus des Menschen (Morphology and topography of human arcus volaris sublimis and profundus) [In German]. Anat Hefte 1897; 7:161-88. http://dx.doi.org/10.1007/BF02298031.
Kachlik D, Konarik M, Horak D, Bernat I, Baca V. Anatomical difficulties of catheterization via arteria radialis. Intervent Akut kardiol 2010; 9:64-8.
Burzotta F, Trani C, De Vita M, Crea F. A new operative classification of both anatomic vascular variants and physiopathologic conditions affecting transradial cardiovascular procedures. Int J Cardiol 2010; 145(1):120-2.
http://dx.doi.org/10.1016/j.ijcard.2009.06.025.
Cohen SM. Accidental intra-arterial injection of drugs. Lancet 1948; 2(6524):409-17. http://dx.doi.org/10.1016/S0140-6736(48)90986-6.
Lister G. The hand: diagnosis and indications. Edinburgh: Churchill Livingstone; 1977. p. 96.
Devansh. Superficial ulnar artery flap. Plast Reconstr Surg 1996; 97(2):420-6. http://dx.doi.org/10.1097/00006534-199602000-00022.
Hazlett JW. The superficial ulnar artery with reference to accidental intra-arterial injection. Can Med Assoc J 1949; 61(3):289-93.
Thoma A, Young JE. The superficial ulnar artery “trap” and the free forearm flap. Ann Plast Surg 1992; 28(4):370-2. http://dx.doi.org/10.1097/00000637-199204000-00013.
Kachlik D, Baca V, Bozdechova I, Cech P, Musil V. Anatomical terminology and nomenclature: past, present and highlights. Surg Radiol Anat 2008; 30(6):459-66. http://dx.doi.org/10.1007/s00276-008-0357-y.
Kachlik D, Bozdechova I, Cech P, Musil V, Baca V. Mistakes in the usage of anatomical terminology in clinical practice. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2009; 153(2):157-61. http://dx.doi.org/10.5507/bp.2009.027.
Kachlik D, Musil V, Baca V. Terminologia anatomica after 17 years: inconsistencies, mistakes, and new proposals. Ann Anat 2015; 201:8-16.
Downloads
Additional Files
Published
How to Cite
Accepted 2015-10-25
Published 2016-03-10









