Investigation of infraclavicular block success using the perfusion index: A randomized clinical trial
DOI:
https://doi.org/10.17305/bjbms.2022.8214Keywords:
Infraclavicular block, perfusion index, peripheral nerve block, brachial plexusAbstract
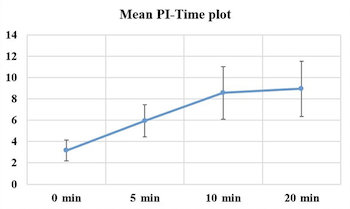
The results of the pinprick and cold tests performed on the arm, forearm, and wrist-wrist areas of patients scheduled for upper extremity procedures are subjective and dependent on patient's compliance. The purpose of this study was to determine whether the perfusion index (PI) could be used as an objective indicator to demonstrate block efficacy. Fifty patients between the ages of 18 and 65 years who were scheduled for upper extremity procedures and had an American Society of Anesthesiologists risk assessment class of I-II were included in this study. Infraclavicular block was performed on the patients using the peripheral nerve stimulation and ultrasonography. Preoperative and postoperative PI values were measured and recorded. The pinprick test took an average of 7.98 ± 1.49 minutes to turn positive, whereas the grade 3 of Modified Bromage Scale took an average of 11.08 ± 1.71 minutes. Differences between baseline values and perioperative values were found to be significantly different in the paired comparisons of the PI values. With 80% sensitivity and 80% specificity, increases in the PI value by or above 3.8 units were indicative for sensory block. With 84% sensitivity and 84% specificity, increases in the PI value by or above 3.9 units were indicative for grade 3 of Modified Bromage Scale in patients. It was determined that the PI is a faster, more reliable, and simpler technique than conventional methods for determining the efficacy of a block because of the vasodilatation that occurs before sensory and motor block.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2022 İbrahim Şeyhanlı, Mehmet Duran, Nezir Yılmaz, Hamza Nakır, Mevlüt Doğukan, Öznur Uludağ

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-10-21
Published 2023-05-01









