Risk factors for recurrent IgA nephropathy after renal transplantation: A meta-analysis
DOI:
https://doi.org/10.17305/bjbms.2022.8369Keywords:
Meta-analysis, IgA nephropathy, kidney transplantation, risk factorsAbstract
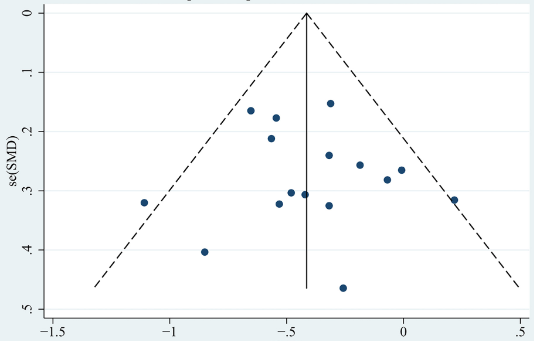
Recurrent glomerulonephritis after renal transplantation is the third most common cause of allograft loss, the most frequent of which is associated with IgA nephropathy (IgAN). This study aims to provide a systematic review of the risk factors associated with recurrent IgAN after renal transplantation. We searched English and Chinese databases, including PubMed, Embase, Web of Science, CNKI, and others, and included all case-control studies involving risk factors for recurrent IgAN after renal transplantation from the databases’ establishment to March 2022. Data were analyzed using the Stata 12.0. A total of 20 case–control studies were included in the meta-analysis, with 542 patients with recurrent IgAN and 1385 patients without recurrent IgAN. The results showed that donor age (standardized mean difference [SMD] -0.13 [95% CI -0.26, -0.001]; P = 0.048), patient age at transplantation (SMD -0.41 [95% CI -0.53, -0.29]; P < 0.001), time from diagnosis to end-stage renal disease (SMD -0.42 [95% CI -0.74, -0.10]; P = 0.010), previous transplantation (odds ratio [OR] 1.73 [95% CI 1.06, 2.81]; P = 0.027), living donor (OR 1.86 [95% CI 1.34, 2.58]; P < 0.001), related donor (OR 2.64, [95% CI 1.84, 3.79]; P < 0.001), tacrolimus use (OR 0.71 [95% CI 0.52, 0.98]; P = 0.035), basiliximab use (OR 0.39 [95% CI 0.27, 0.55]; P < 0.001), proteinuria (SMD 0.42 [95% CI 0.13, 0.71]; P = 0.005) and serum IgA level (SMD 0.48 [95% CI 0.27, 0.69]; P < 0.001) were associated with recurrent IgAN after renal transplantation. In general, tacrolimus and basiliximab use were protective factors against recurrent IgAN after renal transplantation, whereas donor age, patient age at transplantation, time from diagnosis to end-stage renal disease, previous transplantation, living donor, related donor, proteinuria, and serum IgA level were risk factors for recurrent IgAN after renal transplantation. Clinical decision making should warrant further consideration of these risk factors.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2022 Jiang Bai, Qiong Wu, Jing Chen, Zhifang Zheng, Jiarong Chang, Liangliang Wang, Yun Zhou, Qiang Guo

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-11-28
Published 2023-05-01









