Establishment of predictive nomogram and web-based survival risk calculator for desmoplastic small round cell tumor: A propensity score-adjusted, population-based study
DOI:
https://doi.org/10.17305/bb.2022.8633Keywords:
Desmoplastic small round cell tumor (DSRCT), nomogram, survival, triple-therapy, Surveillance, Epidemiology, and End Results (SEER)Abstract
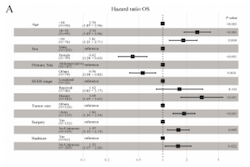
Desmoplastic small round cell tumor (DSRCT) is a rare undifferentiated malignant soft tissue tumor with a poor prognosis and a lack of consensus on treatment. This study’s objective was to build a nomogram based on clinicopathologic factors and an online survival risk calculator to predict patient prognosis and support therapeutic decision-making. A retrospective cohort analysis of the Surveillance, Epidemiology and End Results (SEER) database was performed for patients diagnosed with DSRCT between 2000 and 2019. The least absolute shrinkage and selection operator (LASSO) Cox regression analysis was applied to identify the individual variables related to overall survival (OS) and cancer-specific survival (CSS), as well as to construct online survival risk calculators and nomogram survival models. The nomogram was employed to categorize patients into different risk groups, and the Kaplan-Meier method was utilized to determine the survival rate of each risk category. Propensity score matching (PSM) was used to assess survival with different therapeutic approaches. A total of 374 patients were included, and the median OS and CSS were 25 (interquartile range 21.9-28.1) months and 27 (interquartile range 23.6-30.3) months, respectively. The nomogram models demonstrated high predictive accuracy. PSM found that patients with triple-therapy had better CSS and OS than those who received surgery plus chemotherapy (median survival times: 49 vs 34 months and 49 vs 35 months, respectively). The nomogram successfully predicted the DSRCT patients survival rate. This approach could assist doctors in evaluating prognoses, identifying high-risk populations, and implementing personalized therapy.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2023 Sihao Chen, Yu Pu, Yuzhu Jiang, Yingda Liu, Mengxia Li, Mingfang Xu

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2023-01-03
Published 2023-05-01









