Etiology and clinical features of non-O1/non-O139 Vibrio cholerae infection in an inland city in China
DOI:
https://doi.org/10.17305/bb.2022.8745Keywords:
Non-O1/non-O139 Vibrio cholerae, Vibrio cholerae, infection, bacteremia, antimicrobial susceptibilityAbstract
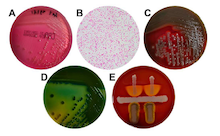
Non-O1/non-O139 Vibrio cholerae (NOVC) causes various illnesses ranging in severity from mild to life-threatening but were ignored previously. Knowledge of the NOVC infection, particularly bacteremia, is limited because of its rarity. Here we first retrospectively reported the demographic, clinical, and therapy characteristics of patients with NOVC infection. Isolated NOVC stains were identified by a series of biochemical, mass spectrometry (MS), and serum agglutination tests. The results of 11 patients with NOVC infection (including 8 with bacteremia) with a median age of 68 years were included in this report. Most isolated NOVC strains had antibiotic susceptibility. Patients with NOVC-positive were distributed in various departments, most occurring in gastroenterology (6 cases). Hepatic disease was the most common comorbid disease, followed by diabetes (3 cases) and biliary tract disease (3 cases). Two cases were previously healthy. The most common symptom at presentation was fever. All patients presented with abnormal changes in hematology and inflammatory parameters. Cephalosporins were the most frequently used antibiotics. Ten patients had a favorable outcome after treatment; one died from complicated underlying diseases. In summary, we recommend the timely identification of NOVC strains using MALDI-TOF-MS. The suspicion of NOVC bacteremia cannot be ruled out regardless of the host’s immune status. An alternative therapeutic regimen for this infection may be β-lactam antibiotics or combined with β-lactamase inhibitors. Regardless, the specific therapeutic regimen should be based on the antibiogram data.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2023 Yu-Han Xiang , Qin-Qin Hu , Yan Liu, Rui Sheng , Jie Wang, Wen-Jing Li, Jian Shi, Xue Li, Shu-Hua Lu

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2023-02-06
Published 2023-07-03









