Interleukin 6 and fetal fibronectin as a predictors of preterm delivery in symptomatic patients
DOI:
https://doi.org/10.17305/bjbms.2015.1.93Keywords:
Preterm labor, fFN, IL-6, predictive valueAbstract
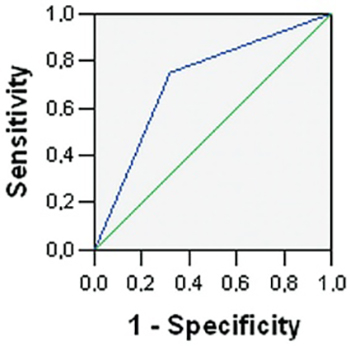
Preterm delivery is the leading cause of neonatal mortality and morbidity. The rate of preterm births has been estimated to be about 15 million, which accounts for 11.1% of all live births worldwide. The purpose of this study was to evaluate the cervico-vaginal (CVF) cytokine IL-6 and fetal fibronectin (fFN) status as predictors of preterm delivery in patients with symptoms of preterm labor. Patients with symptoms suggestive of preterm labor were recruited from September 2013 to March 2014. Vaginal swabs were taken for fetal fibronectin test (fFN) and CVF IL-6. Antibiotics, steroids and tocolytics were administered, where appropriate. The outcome was measured by the occurrence of preterm delivery within 14 days from the day of hospital admission. Cut-off value of 1305 pg/mL for the concentration of IL-6 in the CVF was the best predictor of preterm delivery, with the sensitivity of 69.4% and specificity of 68.2%. Patients with positive fFN test had the OR of 6.429 (95%CI 1.991-20.758) to deliver prematurely. The multivariate analysis of combined fFN and CVF IL-6 tests resulted in risk of 86.7% to deliver prematurely, if both tests were positive. The combination of both tests performed better than the individual tests and decreased the false positive rate, which in turn reduced the chances for inappropriate patient treatment, bringing down the costs.
Citations
Downloads
References
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 2012;379:2162–7.
http://dx.doi.org/10.1016/S0140-6736(12)60820-4
Gyetvai K, Hannah M, Hodnett E, Ohlsson A. Tocolytics for preterm labor: a systematic review. Obstet Gynecol 1999; 94:869–877.
http://dx.doi.org/10.1016/S0029-7844(99)00329-4
King JF, Grant A, Keirse M, Chalmers I. Beta-mimetics in preterm labour: an overview of the randomized controlled trials. Br J Obstet Gynaecol 1988;95:211–222.
http://dx.doi.org/10.1111/j.1471-0528.1988.tb06860.x
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380; 2197–223.
Lockwood CJ, Kuczynski E. Markers of risk for preterm delivery. Perinat Med 1999; 27:5–20.
http://dx.doi.org/10.1515/JPM.1999.001
Mercer BM, Goldenberg RL, Das A, Moawad AH, Iams JD, Meis PJ, et al. The preterm prediction study: a clinical risk assessment system. Am J Obstet Gynecol 1996;174:1885–93
http://dx.doi.org/10.1016/S0002-9378(96)70225-9
Goldenberg RL, Mercer BM, Meis P, Copper R, Das A, McNellis D. The preterm prediction study: fetal fibronectin testing and spontaneous preterm birth. NICHD Maternal Fetal Medicine Units Network. Obstet. Gynaecol 1996;87:643–8
http://dx.doi.org/10.1016/0029-7844(96)00035-X
Lu GC, Goldenberg RL, Cliver SP, Kreaden US, Andrews WW. Vaginal fetal finbronectin levels and spontaneous preterm birth in symptomatic women. Obstet Gynaecol 2001;97:222–8
http://dx.doi.org/10.1016/S0029-7844(00)01130-3
Honest H, Bachmann LM, Gupta JK, Kleijnen J, Khan KS. Accuracy of cervicovaginal fetal fibronectin test in predicting risk of spontaneous preterm birth: systematic review. BMJ 2002;325:301
http://dx.doi.org/10.1136/bmj.325.7359.301
Leitich H, Egarter C, Kaider A, Hohlagschwandtner M, Berghammer P, Husslein P. cervicovaginal fetal fibronectin as a marker for preterm delivery: a meta-analysis. Am. J. Obstet. Gynecol 1999;180: 1169–76.
http://dx.doi.org/10.1016/S0002-9378(99)70612-5
Romero R, Durum S, Dinarello CA, Oyarzun E, Hobbins JC, Mitchell MD. Interleukin-1 stimulates prostaglandin biosynthesis by human amnion. Prostaglandins 1989; 37:13–22.
http://dx.doi.org/10.1016/0090-6980(89)90028-2
Murtha AP, Greig PC, Jimmerson CE, Herbert WN. Maternal serum interleukin-6 concentration as a marker for impending preterm delivery. Obstet Gynecol 1998; 91:161–4.
http://dx.doi.org/10.1016/S0029-7844(97)00602-9
Greig PC, Murtha AP, Jimmerson CJ, Herbert WN, Roitman-Johnson B, Allen J. Maternal serum interleukin-6 during pregnancy and during term and preterm labour. Obstet Gynecol 1997; 90:465–9.
http://dx.doi.org/10.1016/S0029-7844(97)00294-9
Alvarez-de-la-Rosa M, Rebollo FJ, Codoceo R, Gonzalez GA. Maternal serum interleukin 1, 2, 6, 8 and interleukin-2 receptor levels in preterm labor and delivery. Eur J Obstet Gynecol Reprod Biol 2000;88:57–60.
http://dx.doi.org/10.1016/S0301-2115(99)00129-3
Greig PC, Ernest JM, Teot L, Erikson M, Talley R. Amniotic fluid interleukin-6 levels correlate with histologic chorioamnionitis and amniotic fluid cultures in patients in premature labor with intact membranes. Am J Obstet Gynecol 1993; 169:1035–44.
http://dx.doi.org/10.1016/0002-9378(93)90050-S
Maymon E, Ghezzi F, Edwin SS, Mazor M, Yoon BH, Gomez R, et al. The tumor necrosis factor alpha and its soluble receptor profile in term and preterm parturition. Am J Obstet Gynecol 1999; 181:1142–8.
http://dx.doi.org/10.1016/S0002-9378(99)70097-9
Lockwood CJ, Ghidini A, Wein R, Lapinski R, Casal D, Berkowitz RL. Increased interleukin-6 concentrations in cervical secretions are associated with preterm delivery. Am J Obstet Gynecol 1994; 171:1097–102.
http://dx.doi.org/10.1016/0002-9378(94)90043-4
LaShay N, Gilson G, Joffe G, Qualls C, Curet L. Will cervicovaginal interleukin-6 combined with fetal fibronectin testing improve the prediction of preterm delivery? J Matern Fetal Med 2000; 9:336–41.
http://dx.doi.org/10.1002/1520-6661(200011/12)9:6<336::AID-MFM1003>3.0.CO;2-F
Lange M, Chen FK, Wessel J, Buscher U, Dudenhausen JW. Elevation of interleukin-6 levels in cervical secretions as a predictor of preterm delivery. Acta Obstet Gynecol Scand 2003; 82:326–9.
http://dx.doi.org/10.1034/j.1600-0412.2003.00149.x
Grenache DG, Hankins K, Parvin CA, Gronowski AM. Cervicovaginal interleukin-6, tumor necrosis factor-α, and interleukin-2 receptor as markers of preterm delivery. Clin Chem 2004; 50:1839–42.
http://dx.doi.org/10.1373/clinchem.2004.034280
Rozenberg P, Goffinet F, Malagrida L, Giudicelli Y, Perdu M, Houssin I et al. Evaluating the risk of preterm delivery: a comparison of fetal fibronectin and transvaginal ultrasonographic measurement of cervical length. Am J Obstet Gynecol 1997; 176:196–9.
http://dx.doi.org/10.1016/S0002-9378(97)80035-X
Cox SM, ML Casey, PC Macdonald. Accumulation of interleukin-1 beta and interleukin-6 in amniotic fluid: a sequela of labour at term and preterm. Hum Reprod Update 1997; 517-27.
http://dx.doi.org/10.1093/humupd/3.5.517
Garry D, R Figueroa, MA Rosenfeld, E Martinez, P Visintainer, N Tejagani. A comparison of rapid amniotic fluid markers in the prediction of microbial invasion of the uterine cavity and preterm delivery. Am J Obstet Gynecol 1996;1336-41.
http://dx.doi.org/10.1016/S0002-9378(96)70051-0
Gomez R, Ghezzi F, Romero R, Munoz H, Tolosa JE, Rojas I. Premature labor and intra-amniotic infection. Clin Perinatol 1995; 281-342.
Hsu-CD, Meaddough E, Aversa K, Hong SF, Lu LC, Jones DC et al. Elevated amniotic fluid levels of leukemia inhibitory factor, interleukin 6 and interleukin 8 in intra-amniotic infection.Am J Obstet Gynecol 1998; 1267-70.
Murtha AP, PC Greig, CE Jimmerson, WN Herbert. Maternal serum interleukin-6 concentration as a marker of impending preterm delivery. Obstet Gynecol 1998; 161-4.
http://dx.doi.org/10.1016/S0029-7844(97)00602-9
Romero R, M Sirtori, E Oyarzun, et al. Infection and labor: Prevalance, microbiology and clinical significance of intraamniotic infection in women with preterm labor and intact membranes. Am J Obstet Gynecol 1989; 817-24.
http://dx.doi.org/10.1016/0002-9378(89)90409-2
Woodworth A, Moore J, G'Sell C, Verdoes A, Snyder JA, Morris L et al.Diagnostic accuracy of cervicovaginal interleukin-6 and interleukin-6: album in ratio as markers of preterm delivery. Clin Chem 2007; 53:1534-40.
http://dx.doi.org/10.1373/clinchem.2007.084798
Peaceman AM, Andrews WW, Thorp JM, Cliver SP, Lukes A, Iams JD et al. Fetal fibronectin as a predictor of preterm birth in patients with symptoms: a multicenter trial.Am J Obstet Gynecol 1997; 177:13–8.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2014-10-05
Published 2015-01-08









