Comprehensive malnutritional index for predicting clinical outcomes in locally advanced rectal cancer receiving neoadjuvant chemoradiotherapy
DOI:
https://doi.org/10.17305/bb.2024.11188Keywords:
Comprehensive malnutritional index, locally advanced rectal cancer, malnutritional index, neoadjuvant chemoradiotherapy, prognosisAbstract
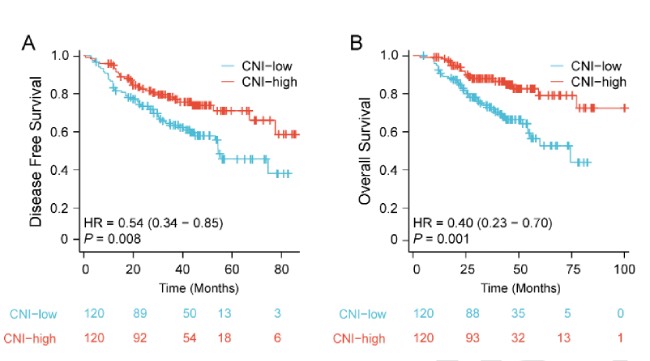
The objective of this investigation was to assess the prognostic significance of the comprehensive malnutritional index (CNI) in patients with locally advanced rectal cancer (LARC) who underwent neoadjuvant chemoradiotherapy (nCRT) followed by surgery. A total of 240 LARC patients were recruited. The CNI was calculated using principal components analysis based on hemoglobin (Hb), total lymphocyte count (TLC), albumin (ALB), body mass index (BMI), and usual body weight percentage (UBW%). The patients were then categorized into two groups based on the median CNI value. Cox regression and survival analyses were performed. The CNI-low (120 cases) and CNI-high (120 cases) groups were classified based on the median CNI value. The results indicated that the CNI demonstrated superior predictive ability for disease-free survival (DFS) and overall survival (OS) compared to other malnutritional indexes. LARC patients in the CNI-high group had significantly longer DFS and OS compared to those in the CNI-low group. Multivariate analysis revealed that the CNI was an independent prognostic factor for DFS (hazard ratio [HR] = 0.49; 95% confidence interval [CI], 0.29–0.83; P = 0.008) and OS (HR = 0.30; 95% CI, 0.16–0.58; P < 0.001). Additionally, the CNI-high group benefited from postoperative chemotherapy (DFS: P = 0.029, OS: P = 0.024), while the CNI-low group did not show such benefits (DFS: P = 0.448, OS: P = 0.468). These findings suggest that the CNI could serve as a valuable prognostic indicator for LARC patients who undergo nCRT followed by surgery. Preoperative nutrition optimization is important for LARC patients.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2024 Yu Xu, Peipei Shen, Jiahao Zhu, Danqi Qian, Ke Gu, Yong Mao, Shengjun Ji, Bo Yang, Yutian Zhao

This work is licensed under a Creative Commons Attribution 4.0 International License.









