Effects of carbamazepine on serum parathormone, 25- hydroxyvitamin D, bone specific alkaline phosphatase, C-telopeptide, and osteocalcin levels in healthy rats
DOI:
https://doi.org/10.17305/bjbms.2012.2445Keywords:
carbamazepine, bone-specific alkaline phosphatase, C-telopeptide, 25-hydroxyvitamin D, osteocalcinAbstract
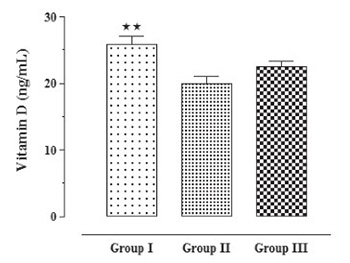
It is still not completely clear whether carbamazepine causes alterations in vitamin D status and in bone metabolism. The objective of this study was to investigate the effects of carbamazepine on serum levels of 25-hydroxyvitamin D and on biomarkers of bone formation and resorption in healthy rats. Levels of calcium, 25-hydroxyvitamin D, parathormone, C-telopeptide, bone specific alkaline phosphatase and osteocalcin were measured in 3 groups of rats consisting of controls (n=10), isotonic saline solution group (n=10) and carbamazepine group (n=10). Mean calcium levels were found to be significantly lower in healthy controls in comparison to isotonic saline solution and carbamazepine groups (10.0±0.24, 10.81±0.16, 10.93±0.22 mg/dL, respectively, p<0.05). Mean levels of 25-hydroxyvitamin D, were found to be significantly higher in control group compared to isotonic saline solution group (25-hydroxyvitamin D; 25.91±1.12, 19.99±0.99 ng/mL, respectively, p<0.01). Mean levels of parathormone and osteocalcin were found to be significantly higher in control group compared to isotonic saline solution group and carbamazepine group. Parathormone levels were measured as 3.46±0.83, 1.08±0.08, 0.94±0.02 pg/mL, respectively (p<0.01). Osteocalcine levels were measured as 1.66±0.001, 1.32±0.002, 1.32±0.001 ng/mL, respectively (p<0.001). A significant difference in terms of mean serum bone specific alkaline phosphatase and C-telopeptide levels among groups was not observed. The main outcome of this prospective study in healthy rats showed no change in biochemical parameters of bone turnover during treatment with carbamazepine.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-09-13
Published 2012-11-20









