Kawasaki-like disease and acute myocarditis in the SARS-CoV-2 pandemic – reports of three adolescents
DOI:
https://doi.org/10.17305/bjbms.2020.5037Keywords:
SARS-CoV-2, myocarditis, Kawasaki disease, adolescent, COVID-19Abstract
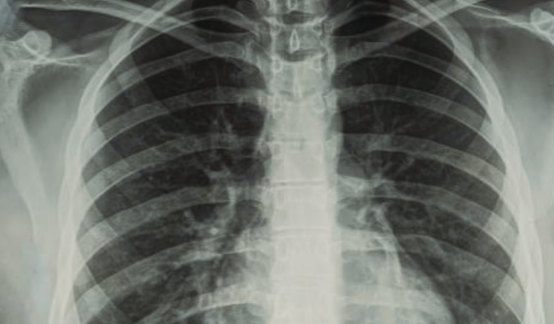
The novel coronavirus disease (COVID-19) may induce multisystem inflammatory syndrome (MIS) in children, which may be associated with Kawasaki-like disease and cardiac injury. In this study, we presented three male adolescents with MIS and myocardial injury admitted to the hospital during the peak of COVID-19 pandemic. All of the three patients had a history of fever, gastrointestinal symptoms, polymorph rash, non-exudative onjunctivitis, and signs of acute myocarditis (AM). One of them had renal failure. Previously, they did not have an acute infection. Upon admission, they were hypotensive and tachycardic. A nasopharyngeal swab for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on reverse transcription-polymerase chain reaction (PCR) assay was negative, but neutralizing viral antibodies were positive. In combination with blood tests, lectrocardiogram, echocardiography, and computerized tomography, a MIS associated with acute myocarditis with mild to moderate systolic dysfunction and dilated coronary arteries were diagnosed. Two of three patients had shock syndrome andrequired inotropic support. All patients were treated with intravenous imunoglobulins (Ig). The second patient had a fever up to 102.2°F (39°C) 3 days after intravenous Ig. Further, he was treated according to protocols for refractory Kawasaki disease, with an intravenous methylprednisolone pulse therapy and aspirin. After a few hours, he became afebrile and the clinical signs disappeared. The favorable short-term
outcome may reflect early recognition and adequate therapy; however, the long-term outcomes are currently unknown.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2020 Stasa Krasic, Sergej Prijic, Predrag Minic, Gordana Petrovic, Dejan Nesic, Vladislav Vukomanovic

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2020-10-10
Published 2021-04-01









