Regulatory aspects of biological medicines in Bosnia and Herzegovina
DOI:
https://doi.org/10.17305/bjbms.2021.6910Keywords:
Original biological medicines (originator biologics), biosimilars, regulatory approach, interchangeability, safetyAbstract
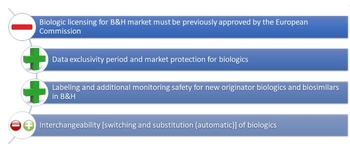
The use of the biological medicines, also called “biologics,” has contributed to the progress of the treatment of many chronic diseases, such as cancer, rheumatoid arthritis, Crohn’s disease, multiple sclerosis, and psoriasis. However, biologicals are expensive for healthcare systems in several countries. Their availability has been a global issue, which has affected many patients that suffer from various diseases. A biosimilar medicine, also called “biosimilar,” is a medicine with similar characteristics in terms of quality, biological activity, safety, and efficacy as the approved original biological medicine, known as “originator biologic.” Biosimilars generate competition within the market because they lower the prices of biologics and thus allow for an increase in patient access. However, there are barriers when it comes to the acceptability rate of biosimilars and how interchangeable they are with the originator biologic. In this review, we present a national regulatory framework for biologics along with its limitations, a system of monitoring the safety profile of biologics, the guideline for interchangeability, and a list of approved and available biologics in Bosnia and Herzegovina. Additionally, recommendations were made here in order to provide opportunities for greater acceptance of biosimilars and better access to biologics. These recommendations include, but are not limited to, strengthening the national regulatory framework for biologics, capacity building, increasing awareness among healthcare providers for reporting adverse drug events and active pharmacovigilance, and better definitions of interchangeability. Finally, awareness among healthcare providers regarding biosimilars and biologics should be raised through continuous education and workshops, and by including this important topic in the graduate and postgraduate curriculum programs in the country.
Citations
Downloads
Downloads
Additional Files
Published
License
Copyright (c) 2022 Biljana Tubic, Saša Jungić

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-02-17
Published 2022-07-29









