Videolaryngoscopy as a primary intubation modality in obstetrics: A narrative review of current evidence
DOI:
https://doi.org/10.17305/bb.2023.9154Keywords:
Videolaryngoscopy, direct laryngoscopy, endotracheal intubation, obstetric anaesthesia, airway managementAbstract
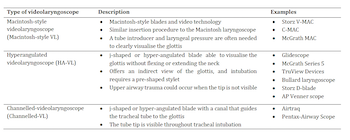
Pregnancy-related physiologic and anatomic changes affect oxygenation and airway management, and it is widely believed that airway difficulty may be more common in obstetric patients as a result. In addition, most obstetric intubations are performed under emergency conditions, and preoperative airway assessment poorly predicts airway management outcomes. These considerations necessitate special protocols for airway care in the obstetric population, and the evolution of the videolaryngoscope represents one of the most important milestones in recent decades. However, recommendations for the use of videolaryngoscopy in obstetrics remain unclear. A considerable body of evidence affirms that videolaryngoscopy improves laryngeal visualisation, increases first-attempt and overall intubation success rates, shortens intubation time, and facilitates team communication and education. In contrast, a significant number of studies have also reported conflicting results regarding comparative clinical outcomes and have highlighted other limitations regarding the adoption of videolaryngoscopy in routine obstetric care. Nevertheless, considering the peculiarities of obstetric intubation, the Macintosh-style videolaryngoscope can be suggested as the primary intubation device as it offers the benefits of both videolaryngoscopy and direct laryngoscopy. However, more rigorous evidence is needed to clarify the current blind spots and controversies regarding the role of videolaryngoscopy in obstetrics.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2023 Tatjana Stopar Pintarič

This work is licensed under a Creative Commons Attribution 4.0 International License.









