ICU admission delays: Impact on length of stay and long-term outcomes
DOI:
https://doi.org/10.17305/bb.2025.12888Keywords:
ICU admission delay, length of stay, Charlson Comorbidity Index, APACHE-II, triage, long-term outcomesAbstract
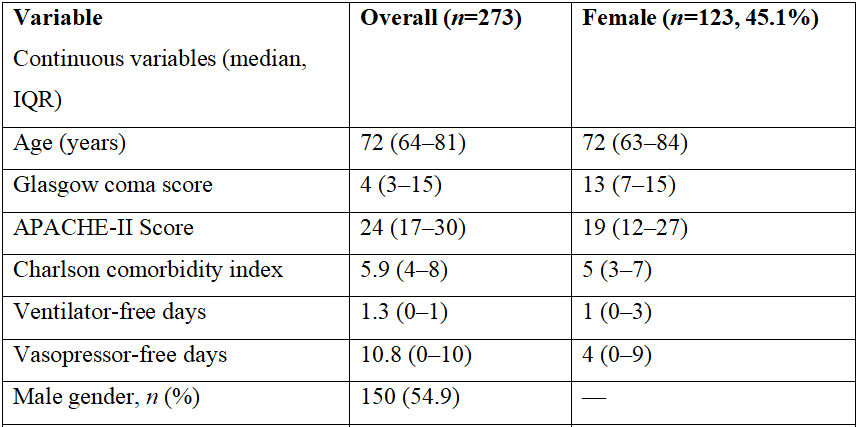
Delays in intensive care unit (ICU) admissions are prevalent in overcrowded hospitals and can adversely affect patient outcomes. However, the extent of this impact, particularly beyond short-term mortality, remains unclear. We hypothesized that ICU admission delays exceeding 6 hours after consultation would independently increase 90-day mortality and prolong ICU length of stay. We conducted a retrospective analysis of data from 273 adult patients admitted to the ICU of a tertiary university hospital between January and December 2019. Patients were stratified into two groups: early admission (≤6 hours) and delayed admission (>6 hours). Multivariate Cox regression was employed to identify independent predictors of mortality. Delayed ICU admission was observed in 72.8% of patients. Although delayed admission was not independently associated with increased mortality in the multivariate analysis (HR: 0.88; 95% CI: 0.61–1.27), it was significantly correlated with prolonged ICU length of stay and higher 90-day mortality in the univariate analysis (p = 0.039), with no significant difference in vasopressor-free days (p = 0.809). In our assessment of independent mortality predictors, we found that patients with higher APACHE-II and Charlson scores experienced longer delays in ICU transfer. Additionally, respiratory and circulatory failure at admission were independently associated with increased mortality (HR: 2.17; 95% CI: 1.51–3.12). While early ICU admission did not independently predict mortality, it was linked to extended ICU stays, an increased treatment burden, and adverse long-term outcomes. These findings underscore the necessity of refining triage processes and evaluating baseline patient severity when interpreting the impact of ICU admission timing on outcomes.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Ferhan Demirer Aydemir, Ozge Kurtkulagi, Bisar Ergun, Vecihe Bayrak, Ozlem Oner, Bilgin Comert, Ali Necati Gokmen, Volkan Hanci

This work is licensed under a Creative Commons Attribution 4.0 International License.









