Advanced immunotherapy across diseases and the role of artificial intelligence: A review
DOI:
https://doi.org/10.17305/bb.2026.13199Keywords:
Immunotherapy, cancer immunotherapy, autoimmune disorders, infectious diseases, artificial intelligenceAbstract
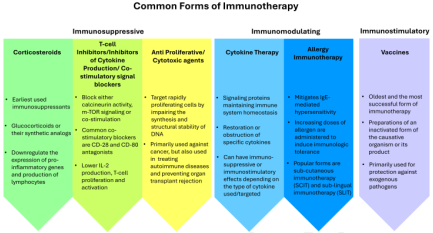
Immunotherapy, a therapeutic strategy aimed at modulating the host immune system, has undergone rapid evolution over recent decades, particularly in oncology. Advanced methodologies, including immune checkpoint inhibition, cytokine therapy, chimeric antigen receptor T-cell therapy (CAR-T), and tumor-infiltrating lymphocyte therapies, have significantly transformed cancer treatment. This review summarizes recent advancements in immunotherapy and examines its expanding applications across a range of diseases, such as autoimmune disorders, infectious diseases, transplant rejection, and allergic conditions. A structured literature search was conducted using PubMed and Google Scholar, prioritizing studies published from 2015 to 2026. The findings underscore the efficacy of monoclonal antibodies, adoptive cell therapies, cytokine modulation, and checkpoint-targeted strategies beyond oncology. However, challenges remain, including variable patient responses, immune-related adverse events, and treatment costs. This review also explores the emerging role of artificial intelligence (AI) in enhancing personalized immunotherapy through patient stratification, biomarker identification, and predictive modeling. The integration of multi-omics data with AI presents promising opportunities for improving treatment efficacy and safety, although issues related to data quality, interpretability, regulatory frameworks, and ethical considerations must be addressed. In conclusion, immunotherapy is rapidly extending beyond cancer, and AI-supported personalized approaches offer a promising pathway to safer, more effective, and broadly applicable treatments.
Citations
Downloads
References
Kulwal V, Sawarkar S. Immunotherapy: A concept. JIANFOMT. 2021:1–19.
https://doi.org/10.1007/978-981-15-9038-2_1
Eno JJ. Immunotherapy through the years. JOTAPIO. 2017;8(7):747.
https://doi.org/10.6004/jadpro.2017.8.7.8
Araki K, Maeda R. A brief chronicle of antibody research and technological advances. Antibodies. 2024;13(4):90.
https://doi.org/10.3390/antib13040090
Kaufmann SH. Immunology’s coming of age. FII. 2019;10:453189.
https://doi.org/10.3389/fimmu.2019.00684
Gross L. Intradermal immunization of C3H mice against a sarcoma that originated in an animal of the same line. Cancer Res. 1943;3(5):326–33.
Foley EJ. Antigenic properties of methylcholanthrene-induced tumors in mice of the strain of origin. Cancer Res. 1953;13(12):835–7.
Prehn RT, Main JM. Immunity to methylcholanthrene-induced sarcomas. J Natl Cancer Inst. 1957;18(6):769–78.
Thomas L, Lawrence H. Cellular and humoral aspects of the hypersensitive states. NYH-H. 1959:529–32.
Burnet M. Cancer—a biological approach: III. Viruses associated with neoplastic conditions. IV. Practical applications. BMJ. 1957;1(5023):841.
https://doi.org/10.1136/bmj.1.5023.841
Burnet F. The concept of immunological surveillance. Immunology (Acta/Ann). 1970;13:1–27.
https://doi.org/10.1159/000386035
Allison J. A brief history of immunotherapy. JTO. 2014;3.
Allison JP, McIntyre BW, Bloch D. Tumor-specific antigen of murine T-lymphoma defined with monoclonal antibody. J Immunol. 1982;129(5):2293–300.
https://doi.org/10.4049/jimmunol.129.5.2293
Shi Y, Strasser A, Green DR, Latz E, Mantovani A, Melino G, et al. Legacy of the discovery of the T-cell receptor: 40 years of shaping basic immunology and translational work to develop novel therapies. Cell. 2024;21(7):790–7.
https://doi.org/10.1038/s41423-024-01168-4
Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T-cell basic science to clinical practice. Nat Rev Immunol. 2020;20(11):651–68.
https://doi.org/10.1038/s41577-020-0306-5
Dobosz P, Dzieciątkowski T. The intriguing history of cancer immunotherapy. FII. 2019;10:496087.
https://doi.org/10.3389/fimmu.2019.02965
Durham SR, Shamji MH. Allergen immunotherapy: past, present and future. Nat Rev Immunol. 2023;23(5):317–28.
https://doi.org/10.1038/s41577-022-00786-1
Bucktrout SL, Bluestone JA, Ramsdell F. Recent advances in immunotherapies: from infection and autoimmunity, to cancer, and back again. Genome Med. 2018;10(1):79.
https://doi.org/10.1186/s13073-018-0588-4
Naran K, Nundalall T, Chetty S, Barth S. Principles of immunotherapy: implications for treatment strategies in cancer and infectious diseases. Front Microbiol. 2018;9:405758.
https://doi.org/10.3389/fmicb.2018.03158
Mahoney KM, Rennert PD, Freeman GJ. Combination cancer immunotherapy and new immunomodulatory targets. Nat Rev Drug Discov. 2015;14(8):561–84.
https://doi.org/10.1038/nrd4591
Ma W, Xue R, Zhu Z, Farrukh H, Song W, Li T, et al. Increasing cure rates of solid tumors by immune checkpoint inhibitors. Signal Transduct Target Ther. 2023;12(1):10.
https://doi.org/10.1186/s40164-023-00372-8
Varadé J, Magadán S, González-Fernández Á. Human immunology and immunotherapy: main achievements and challenges. CMI. 2021;18(4):805–28.
https://doi.org/10.1038/s41423-020-00530-6
Sun Q, Hong Z, Zhang C, Wang L, Han Z, Ma D, et al. Immune checkpoint therapy for solid tumours: clinical dilemmas and future trends. Sig Transduct Target Ther. 2023;8(1):320.
https://doi.org/10.1038/s41392-023-01522-4
Propper DJ, Balkwill FR. Harnessing cytokines and chemokines for cancer therapy. Nat Rev Clin Oncol. 2022;19(4):237–53.
https://doi.org/10.1038/s41571-021-00588-9
MRCRCC Trial (Lancet). Interferon-α and survival in metastatic renal carcinoma: early results of a randomised controlled trial. Lancet. 1999;353(9146):14–7.
https://doi.org/10.1016/S0140-6736(98)03544-2
Chamie K, Chang SS, Kramolowsky E, Gonzalgo ML, Agarwal PK, Bassett JC, et al. IL-15 superagonist NAI in BCG-unresponsive non-muscle-invasive bladder cancer. NEJM Evidence. 2022;2(1):EVIDoa2200167.
https://doi.org/10.1056/EVIDoa2200167
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–22.
https://doi.org/10.1056/NEJMoa1001294
Pallerla S, Abdul AuRM, Comeau J, Jois S. Cancer vaccines, treatment of the future: with emphasis on HER2-positive breast cancer. Int J Mol Sci. 2021;22(2):779.
https://doi.org/10.3390/ijms22020779
Ejaz M, Syed MA. Therapeutic cancer vaccines; past, present, and future aspects. HOC Immunology. Springer. 2022:1–21.
https://doi.org/10.1007/978-3-030-80962-1_207-1
Lin MJ, Svensson-Arvelund J, Lubitz GS, Marabelle A, Melero I, Brown BD, et al. Cancer vaccines: the next immunotherapy frontier. Nat Cancer. 2022;3(8):911–26.
https://doi.org/10.1038/s43018-022-00418-6
Lovatt C, Parker AL. Oncolytic viruses and immune checkpoint inhibitors: the “hot” new power couple. Cancers. 2023;15(16):4178.
https://doi.org/10.3390/cancers15164178
Zhao Y, Deng J, Rao S, Guo S, Shen J, Du F, et al. Tumor-infiltrating lymphocyte (TIL) therapy for solid tumor treatment: progressions and challenges. Cancers. 2022;14(17):4160.
https://doi.org/10.3390/cancers14174160
Rohaan MW, van den Berg JH, Kvistborg P, Haanen J. Adoptive transfer of tumor-infiltrating lymphocytes in melanoma: a viable treatment option. J Immunother Cancer. 2018;6(1):102.
https://doi.org/10.1186/s40425-018-0391-1
Thirumalaisamy R, Vasuki S, Sindhu S, Mothilal T, Srimathi V, Poornima B, et al. FDA-approved chimeric antigen receptor (CAR)-T cell therapy for different cancers—a recent perspective. Mol Biotechnol. 2025;67(2):469–83.
https://doi.org/10.1007/s12033-024-01090-0
Zheng Z, Li S, Liu M, Chen C, Zhang L, Zhou D. Fine-tuning through generations: advances in structure and production of CAR-T therapy. Cancers. 2023;15(13):3476.
https://doi.org/10.3390/cancers15133476
Chandrashekara S. The treatment strategies of autoimmune disease may need a different approach from conventional protocol: a review. Indian J Pharmacol. 2012;44(6):665–71.
https://doi.org/10.4103/0253-7613.103235
Ruperto N, Lovell DJ, Quartier P, Paz E, Rubio-Pérez N, Silva CA, et al. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372(9636):383–91.
https://doi.org/10.1016/S0140-6736(08)60998-8
Rachid O, Osman A, Abdi R, Haik Y. CTLA4-Ig (abatacept): a promising investigational drug for use in type 1 diabetes. Expert Opin Investig Drugs. 2020;29(3):221–36.
https://doi.org/10.1080/13543784.2020.1727885
Orban T, Bundy B, Becker DJ, DiMeglio LA, Gitelman SE, Goland R, et al. Co-stimulation modulation with abatacept in patients with recent-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. Lancet. 2011;378(9789):412–19.
https://doi.org/10.1016/S0140-6736(11)60886-6
Russell WE, Bundy BN, Anderson MS, Cooney LA, Gitelman SE, Goland RS, et al. Abatacept for delay of type 1 diabetes progression in stage 1 relatives at risk: a randomized, double-masked, controlled trial. Diabetes Care. 2023;46(5):1005–13.
https://doi.org/10.2337/dci23-0050
Siddiqui Z, Tedesco-Silva H, Riella LV. Belatacept in kidney transplantation—past and future perspectives. Braz J Nephrol. 2017;39:205–12.
https://doi.org/10.5935/0101-2800.20170035
Tuttle J, Drescher E, Simón-Campos JA, Emery P, Greenwald M, Kivitz A, et al. A phase 2 trial of peresolimab for adults with rheumatoid arthritis. New England Journal of Medicine. 2023;388(20):1853–62.
https://doi.org/10.1056/NEJMoa2209856
Klatzmann D, Abbas AK. The promise of low-dose interleukin-2 therapy for autoimmune and inflammatory diseases. Nature Reviews Immunology. 2015;15(5):283–94.
https://doi.org/10.1038/nri3823
Harris F, Berdugo YA, Tree T. IL-2-based approaches to Treg enhancement. Clinical and Experimental Immunology. 2023;211(2):149–63.
https://doi.org/10.1093/cei/uxac105
Filipi M, Jack S. Interferons in the treatment of multiple sclerosis: a clinical efficacy, safety, and tolerability update. International Journal of MS Care. 2020;22(4):165–72.
https://doi.org/10.7224/1537-2073.2018-063
Postal M, Vivaldo JF, Fernandez-Ruiz R, Paredes JL, Appenzeller S, Niewold TB. Type I interferon in the pathogenesis of systemic lupus erythematosus. Current Opinion in Immunology. 2020;67:87–94.
https://doi.org/10.1016/j.coi.2020.10.014
Burki TK. FDA approval for anifrolumab in patients with lupus. The Lancet Rheumatology. 2021;3(10):e689.
https://doi.org/10.1016/S2665-9913(21)00291-5
Jung SM, Kim W-U. Targeted immunotherapy for autoimmune disease. Immune Network. 2022;22(1):e9.
https://doi.org/10.4110/in.2022.22.e9
Marinho A, Delgado Alves J, Fortuna J, Faria R, Almeida I, Alves G, et al. Biological therapy in systemic lupus erythematosus, antiphospholipid syndrome, and Sjögren's syndrome: Evidence- and practice-based guidance. Frontiers in Immunology. 2023;14:1117699.
https://doi.org/10.3389/fimmu.2023.1117699
Ellebrecht CT, Bhoj VG, Nace A, Choi EJ, Mao X, Cho MJ, et al. Reengineering chimeric antigen receptor T cells for targeted therapy of autoimmune disease. Science. 2016;353(6295):179–84.
https://doi.org/10.1126/science.aaf6756
Li Y-R, Lyu Z, Chen Y, Fang Y, Yang L. Frontiers in CAR-T cell therapy for autoimmune diseases. Trends in Pharmacological Sciences. 2024.
https://doi.org/10.1016/j.tips.2024.07.005
Yeh W-I, Seay HR, Newby B, Posgai AL, Moniz FB, Michels A, et al. Avidity and bystander suppressive capacity of human regulatory T cells expressing de novo autoreactive T-cell receptors in type 1 diabetes. Frontiers in Immunology. 2017;8:1313.
https://doi.org/10.3389/fimmu.2017.01313
Randall KL. Rituximab in autoimmune diseases. Australian Prescriber. 2016;39(4):131.
https://doi.org/10.18773/austprescr.2016.053
Blair HA, Duggan ST. Belimumab: a review in systemic lupus erythematosus. Drugs. 2018;78:355–66.
https://doi.org/10.1007/s40265-018-0872-z
Fiyouzi T, Pelaez-Prestel HF, Reyes-Manzanas R, Lafuente EM, Reche PA. Enhancing regulatory T cells to treat inflammatory and autoimmune diseases. International Journal of Molecular Sciences. 2023;24(9):7797.
https://doi.org/10.3390/ijms24097797
Kohm AP, Carpentier PA, Anger HA, Miller SD. Cutting edge: CD4+ CD25+ regulatory T cells suppress antigen-specific autoreactive immune responses and central nervous system inflammation during active experimental autoimmune encephalomyelitis. Journal of Immunology. 2002;169(9):4712–6.
https://doi.org/10.4049/jimmunol.169.9.4712
Fransson M, Piras E, Burman J, Nilsson B, Essand M, Lu B, et al. CAR/FoxP3-engineered T regulatory cells target the CNS and suppress EAE upon intranasal delivery. Journal of Neuroinflammation. 2012;9:1–12.
https://doi.org/10.1186/1742-2094-9-112
Scalapino KJ, Tang Q, Bluestone JA, Bonyhadi ML, Daikh DI. Suppression of disease in New Zealand Black/New Zealand White lupus-prone mice by adoptive transfer of ex vivo expanded regulatory T cells. Journal of Immunology. 2006;177(3):1451–9.
https://doi.org/10.4049/jimmunol.177.3.1451
Weigert O, von Spee C, Undeutsch R, Kloke L, Humrich JY, Riemekasten G, et al. CD4+ Foxp3+ regulatory T cells prolong drug-induced disease remission in (NZBxNZW) F1 lupus mice. Arthritis Research & Therapy. 2013;15:1–11.
https://doi.org/10.1186/ar4188
Tang Q, Henriksen KJ, Bi M, Finger EB, Szot G, Ye J, et al. In vitro-expanded antigen-specific regulatory T cells suppress autoimmune diabetes. Journal of Experimental Medicine. 2004;199(11):1455–65.
https://doi.org/10.1084/jem.20040139
Zhang L, Sosinowski T, Cox AR, Cepeda JR, Sekhar NS, Hartig SM, et al. Chimeric antigen receptor (CAR) T cells targeting a pathogenic MHC class II: peptide complex modulate the progression of autoimmune diabetes. Journal of Autoimmunity. 2019;96:50–8.
https://doi.org/10.1016/j.jaut.2018.08.004
Tenspolde M, Zimmermann K, Weber LC, Hapke M, Lieber M, Dywicki J, et al. Regulatory T cells engineered with a novel insulin-specific chimeric antigen receptor as a candidate immunotherapy for type 1 diabetes. Journal of Autoimmunity. 2019;103:102289.
https://doi.org/10.1016/j.jaut.2019.05.017
Kinnear G, Jones ND, Wood KJ. Costimulation blockade: current perspectives and implications for therapy. Transplantation. 2013;95(4):527–35.
https://doi.org/10.1097/TP.0b013e31826d4672
Ding M, He Y, Zhang S, Guo W. Recent advances in costimulatory blockade to induce immune tolerance in liver transplantation. Frontiers in Immunology. 2021;12:537079.
https://doi.org/10.3389/fimmu.2021.537079
Kitchens WH, Larsen CP, Badell IR. Costimulatory blockade and solid organ transplantation: the past, present and future. Kidney International Reports. 2023.
https://doi.org/10.1016/j.ekir.2023.08.037
Ramamurthy D, Nundalall T, Cingo S, Mungra N, Karaan M, Naran K, et al. Recent advances in immunotherapies against infectious diseases. Immunotherapy Advances. 2021;1(1):ltaa007.
https://doi.org/10.1093/immadv/ltaa007
Seif M, Einsele H, Löffler J. CAR T cells beyond cancer: hope for immunomodulatory therapy of infectious diseases. Frontiers in Immunology. 2019;10:498743.
https://doi.org/10.3389/fimmu.2019.02711
Leibman RS, Richardson MW, Ellebrecht CT, Maldini CR, Glover JA, Secreto AJ, et al. Supraphysiologic control over HIV-1 replication mediated by CD8 T cells expressing a re-engineered CD4-based chimeric antigen receptor. PLOS Pathogens. 2017;13(10):e1006613.
https://doi.org/10.1371/journal.ppat.1006613
Wang X, Liu J, Hao F, Ajavavarakula T, Shi X. CAR-T therapy in HIV: pioneering advances and navigating challenges. Infectious Diseases & Immunity. 2024;4(04):194–205.
https://doi.org/10.1097/ID9.0000000000000129
Otsubo R, Yasui T. Monoclonal antibody therapeutics for infectious diseases: beyond normal human immunoglobulin. Pharmacology & Therapeutics. 2022;240:108233.
https://doi.org/10.1016/j.pharmthera.2022.108233
Miljanovic D, Cirkovic A, Lazarevic I, Knezevic A, Cupic M, Banko A, et al. Clinical efficacy of anti‐SARS‐CoV‐2 monoclonal antibodies in preventing hospitalisation and mortality among patients infected with Omicron variants: a systematic review and meta‐analysis. Reviews in Medical Virology. 2023;33(4):e2439.
https://doi.org/10.1002/rmv.2439
Cox M, Peacock TP, Harvey WT, Hughes J, Wright DW, Willett BJ, et al. SARS-CoV-2 variant evasion of monoclonal antibodies based on in vitro studies. Nature Reviews Microbiology. 2023;21(2):112–24.
https://doi.org/10.1038/s41579-022-00809-7
Fausther-Bovendo H, Kobinger G. The road to effective and accessible antibody therapies against Ebola virus. Current Opinion in Virology. 2022;54:101210.
https://doi.org/10.1016/j.coviro.2022.101210
Promsote W, DeMouth ME, Almasri CG, Pegu A. Anti-HIV-1 antibodies: an update. BioDrugs. 2020;34(2):121–32.
https://doi.org/10.1007/s40259-020-00413-2
Walter EB, Munoz FM. New approaches to respiratory syncytial virus prevention and treatment. Annual Review of Medicine. 2025;76.
https://doi.org/10.1146/annurev-med-061323-073934
Rijal P, Donnellan FR. A review of broadly protective monoclonal antibodies to treat Ebola virus disease. Current Opinion in Virology. 2023;61:101339.
https://doi.org/10.1016/j.coviro.2023.101339
Wang C-Y, Wong W-W, Tsai H-C, Chen Y-H, Kuo B-S, Lynn S, et al. Effect of anti-CD4 antibody UB-421 on HIV-1 rebound after treatment interruption. New England Journal of Medicine. 2019;380(16):1535–45.
https://doi.org/10.1056/NEJMoa1802264
Verma V. Leveraging monoclonal antibodies as therapeutics to address antimicrobial resistance in bacteria. Journal of Applied Biology & Biotechnology. 2023;11(3):53–60.
https://doi.org/10.7324/JABB.2023.90087
Kharga K, Kumar L, Patel SKS, Lazarevic I, Knezevic A, Cupic M, et al. Recent advances in monoclonal antibody-based approaches in the management of bacterial sepsis. Biomedicines. 2023;11(3):765.
https://doi.org/10.3390/biomedicines11030765
Hesse EM, Godfred-Cato S, Bower WA. Antitoxin use in the prevention and treatment of anthrax disease: a systematic review. Clinical Infectious Diseases. 2022;75(Supplement_3):S432–S40.
https://doi.org/10.1093/cid/ciac532
Mohamed MF, Ward C, Beran A, Abdallah MA, Asemota J, Kelly CR. Efficacy, safety, and cost-effectiveness of bezlotoxumab in preventing recurrent Clostridioides difficile infection: systematic review and meta-analysis. Journal of Clinical Gastroenterology. 2024;58(4):389–401.
https://doi.org/10.1097/MCG.0000000000001875
Laustsen AH. How can monoclonal antibodies be harnessed against neglected tropical diseases and other infectious diseases? Expert Opinion on Drug Discovery. 2019;14(11):1103–12.
https://doi.org/10.1080/17460441.2019.1646723
Aleshnick M, Florez-Cuadros M, Martinson T, Wilder BK. Monoclonal antibodies for malaria prevention. Molecular Therapy. 2022;30(5):1810–21.
https://doi.org/10.1016/j.ymthe.2022.04.001
Lyke KE, Berry AA, Mason K, Idris AH, O'Callahan M, Happe M, et al. Low-dose intravenous and subcutaneous CIS43LS monoclonal antibody for protection against malaria (VRC 612 Part C): a phase 1, adaptive trial. The Lancet Infectious Diseases. 2023;23(5):578–88.
van der Boor SC, Smit MJ, van Beek SW, Ramjith J, Teelen K, van de Vegte-Bolmer M, et al. Safety, tolerability, and Plasmodium falciparum transmission-reducing activity of monoclonal antibody TB31F: a single-centre, open-label, first-in-human, dose-escalation, phase 1 trial in healthy malaria-naive adults. The Lancet Infectious Diseases. 2022;22(11):1596–605.
https://doi.org/10.1016/S1473-3099(22)00428-5
Wykes MN, Lewin SR. Immune checkpoint blockade in infectious diseases. Nature Reviews Immunology. 2018;18(2):91–104.
https://doi.org/10.1038/nri.2017.112
Porichis F, Kwon DS, Zupkosky J, Tighe DP, McMullen A, Brockman MA, et al. Responsiveness of HIV-specific CD4 T cells to PD-1 blockade. Blood. 2011;118(4):965–74.
https://doi.org/10.1182/blood-2010-12-328070
Chew GM, Fujita T, Webb GM, Burwitz BJ, Wu HL, Reed JS, et al. TIGIT marks exhausted T cells, correlates with disease progression, and serves as a target for immune restoration in HIV and SIV infection. PLOS Pathogens. 2016;12(1):e1005349.
https://doi.org/10.1371/journal.ppat.1005349
Rasmussen TA, McMahon J, Chang JJ, Symons J, Roche M, Dantanarayana A, et al. Impact of alemtuzumab on HIV persistence in an HIV-infected individual on antiretroviral therapy with Sezary syndrome. AIDS. 2017;31(13):1839–45.
https://doi.org/10.1097/QAD.0000000000001540
Gay CL, Bosch RJ, Ritz J, Hataye JM, Aga E, Tressler RL, et al. Clinical trial of the anti-PD-L1 antibody BMS-936559 in HIV-1 infected participants on suppressive antiretroviral therapy. Journal of Infectious Diseases. 2017;215(11):1725–33.
https://doi.org/10.1093/infdis/jix191
Gardiner D, Lalezari J, Lawitz E, DiMicco M, Ghalib R, Reddy KR, et al. A randomized, double-blind, placebo-controlled assessment of BMS-936558, a fully human monoclonal antibody to programmed death-1 (PD-1), in patients with chronic hepatitis C virus infection. PLOS ONE. 2013;8(5):e63818.
https://doi.org/10.1371/journal.pone.0063818
Gane E, Gaggar A, Nguyen A, Subramanian G, McHutchison J, Schwabe C, et al. A phase 1 study evaluating anti-PD-1 treatment with or without GS-4774 in HBeAg-negative chronic hepatitis B patients. Journal of Hepatology. 2017;66(S1):S26–S7.
https://doi.org/10.1016/S0168-8278(17)30315-X
Yau T, Kang Y-K, Kim T-Y, El-Khoueiry AB, Santoro A, Sangro B, et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the CheckMate 040 randomized clinical trial. JAMA Oncology. 2020;6(11):e204564–e.
https://doi.org/10.1001/jamaoncol.2020.4564
Barber DL, Sakai S, Kudchadkar RR, Fling SP, Day TA, Vergara JA, et al. Tuberculosis following PD-1 blockade for cancer immunotherapy. Science Translational Medicine. 2019;11(475):eaat2702.
https://doi.org/10.1126/scitranslmed.aat2702
Lázár-Molnár E, Chen B, Sweeney KA, Wang EJ, Liu W, Lin J, et al. Programmed death-1 (PD-1)-deficient mice are extraordinarily sensitive to tuberculosis. Proceedings of the National Academy of Sciences of the USA. 2010;107(30):13402–7.
https://doi.org/10.1073/pnas.1007394107
Anand K, Sahu G, Burns E, Ensor A, Ensor J, Pingali SR, et al. Mycobacterial infections due to PD-1 and PD-L1 checkpoint inhibitors. ESMO Open. 2020;5(4):e000866.
https://doi.org/10.1136/esmoopen-2020-000866
Jayaraman P, Jacques MK, Zhu C, Steblenko KM, Stowell BL, Madi A, et al. TIM3 mediates T cell exhaustion during Mycobacterium tuberculosis infection. PLOS Pathogens. 2016;12(3):e1005490.
https://doi.org/10.1371/journal.ppat.1005490
Phillips BL, Gautam US, Bucsan AN, Foreman TW, Golden NA, Niu T, et al. LAG-3 potentiates the survival of Mycobacterium tuberculosis in host phagocytes by modulating mitochondrial signaling in an in-vitro granuloma model. PLOS ONE. 2017;12(9):e0180413.
https://doi.org/10.1371/journal.pone.0180413
Vaddi A, Hulsebus HJ, O'Neill EL, Knight V, Chan ED. A narrative review of the controversy on the risk of mycobacterial infections with immune checkpoint inhibitor use: does Goldilocks have the answer? Journal of Thoracic Disease. 2024;16(2):1601.
https://doi.org/10.21037/jtd-23-1395
Lyu J, Narum DE, Baldwin SL, Larsen SE, Bai X, Griffith DE, et al. Understanding the development of tuberculous granulomas: insights into host protection and pathogenesis, a review in humans and animals. Frontiers in Immunology. 2024;15:1427559.
https://doi.org/10.3389/fimmu.2024.1427559
da Fonseca-Martins AM, Ramos TD, Pratti JE, Firmino-Cruz L, Gomes DCO, Soong L, et al. Immunotherapy using anti-PD-1 and anti-PD-L1 in Leishmania amazonensis-infected BALB/c mice reduce parasite load. Scientific Reports. 2019;9(1):20275.
https://doi.org/10.1038/s41598-019-56336-8
Liang SC, Greenwald RJ, Latchman YE, Rosas L, Satoskar A, Freeman GJ, et al. PD‐L1 and PD‐L2 have distinct roles in regulating host immunity to cutaneous leishmaniasis. European Journal of Immunology. 2006;36(1):58–64.
https://doi.org/10.1002/eji.200535458
Kumar R, Chauhan SB, Ng SS, Sundar S, Engwerda CR. Immune checkpoint targets for host-directed therapy to prevent and treat leishmaniasis. Frontiers in Immunology. 2017;8:1492.
https://doi.org/10.3389/fimmu.2017.01492
Butler NS, Moebius J, Pewe LL, Traore B, Doumbo OK, Tygrett LT, et al. Therapeutic blockade of PD-L1 and LAG-3 rapidly clears established blood-stage Plasmodium infection. Nature Immunology. 2012;13(2):188–95.
https://doi.org/10.1038/ni.2180
Hou N, Zou Y, Piao X, Liu S, Wang L, Li S, et al. T-cell immunoglobulin- and mucin-domain-containing molecule 3 signaling blockade improves cell-mediated immunity against malaria. Journal of Infectious Diseases. 2016;214(10):1547–56.
https://doi.org/10.1093/infdis/jiw428
Hafalla JCR, Claser C, Couper KN, Grau GE, Renia L, de Souza JB, et al. The CTLA-4 and PD-1/PD-L1 inhibitory pathways independently regulate host resistance to Plasmodium-induced acute immune pathology. PLOS Pathogens. 2012;8(2):e1002504.
https://doi.org/10.1371/journal.ppat.1002504
Zheng H, Zhang Y, Pan J, Liu N, Qin Y, Qiu L, et al. The role of type 2 innate lymphoid cells in allergic diseases. Frontiers in Immunology. 2021;12:586078.
https://doi.org/10.3389/fimmu.2021.586078
Pengo N, Wuillemin N, Bieli D, Gasser P. Anti-allergen monoclonal antibodies for the treatment of allergies. Allergo Journal International. 2023;32(7):289–95.
https://doi.org/10.1007/s40629-023-00263-8
Bernstein ZJ, Shenoy A, Chen A, Heller NM, Spangler JB. Engineering the IL‐4/IL‐13 axis for targeted immune modulation. Immunological Reviews. 2023;320(1):29–57.
https://doi.org/10.1111/imr.13230
Slager RE, Otulana BA, Hawkins GA, Yen YP, Peters SP, Wenzel SE, et al. IL-4 receptor polymorphisms predict reduction in asthma exacerbations during response to an anti-IL-4 receptor α antagonist. Journal of Allergy and Clinical Immunology. 2012;130(2):516–22.e4.
https://doi.org/10.1016/j.jaci.2012.03.030
Chen Y, Wang W, Yuan H, Li Y, Lv Z, Cui Y, et al. Current state of monoclonal antibody therapy for allergic diseases. Engineering. 2021;7(11):1552–6.
https://doi.org/10.1016/j.eng.2020.06.029
Ali T, Jawed I, Maqsood B, Khan I, Haque MA. Xolair (omalizumab) breakthrough: FDA's first approval to combat allergic reactions to multiple foods. JIGH. 2025;e00554.
https://doi.org/10.1097/GH9.0000000000000554
Gauvreau GM, Arm JP, Boulet L-P, Leigh R, Cockcroft DW, Davis BE, et al. Efficacy and safety of multiple doses of QGE031 (ligelizumab) versus omalizumab and placebo in inhibiting allergen-induced early asthmatic responses. Journal of Allergy and Clinical Immunology. 2016;138(4):1051–9.
https://doi.org/10.1016/j.jaci.2016.02.027
Maurer M, Ensina LF, Gimenez-Arnau AM, Sussman G, Hide M, Saini S, et al. Efficacy and safety of ligelizumab in adults and adolescents with chronic spontaneous urticaria: results of two phase 3 randomised controlled trials. The Lancet. 2024;403(10422):147–59.
Kuo B-S, Li C-H, Chen J-B, Shiung Y-Y, Chu C-Y, Lee C-H, et al. IgE-neutralizing UB-221 mAb, distinct from omalizumab and ligelizumab, exhibits CD23-mediated IgE downregulation and relieves urticaria symptoms. Journal of Clinical Investigation. 2023;132(15).
https://doi.org/10.1172/JCI157765
Strowd LC, Feldman SR. Dupilumab for atopic dermatitis. The Lancet. 2017;389(10086):2265–6.
https://doi.org/10.1016/S0140-6736(17)31192-3
Napolitano M, Fabbrocini G, Neri I, Stingeni L, Boccaletti V, Piccolo V, et al. Dupilumab treatment in children aged 6–11 years with atopic dermatitis: a multicentre, real-life study. Paediatric Drugs. 2022;24(6):671–8.
https://doi.org/10.1007/s40272-022-00531-0
Dodson J, Lio PA. Biologics and small molecule inhibitors: an update in therapies for allergic and immunologic skin diseases. Current Allergy and Asthma Reports. 2022;22(12):183–93.
https://doi.org/10.1007/s11882-022-01047-w
Skuljec J, Chmielewski M, Happle C, Habener A, Busse M, Abken H, et al. Chimeric antigen receptor-redirected regulatory T cells suppress experimental allergic airway inflammation, a model of asthma. Frontiers in Immunology. 2017;8:247521.
https://doi.org/10.3389/fimmu.2017.01125
Esmaeilzadeh A, Tahmasebi S, Athari SS. Chimeric antigen receptor-T cell therapy: applications and challenges in treatment of allergy and asthma. Biomedicine & Pharmacotherapy. 2020;123:109685.
https://doi.org/10.1016/j.biopha.2019.109685
Ward DE, Fay BL, Adejuwon A, Han H, Ma Z. Chimeric antigen receptors based on low affinity mutants of FcεRI re-direct T cell specificity to cells expressing membrane IgE. Frontiers in Immunology. 2018;9:2231.
https://doi.org/10.3389/fimmu.2018.02231
Morita H, Saito H, Matsumoto K. Immune checkpoint molecules on ILC2s as potential therapeutic targets for allergic diseases. Journal of Allergy and Clinical Immunology. 2022;149(1):60–2.
https://doi.org/10.1016/j.jaci.2021.10.021
Helou DG, Shafiei-Jahani P, Lo R, Howard E, Hurrell BP, Galle-Treger L, et al. PD-1 pathway regulates ILC2 metabolism and PD-1 agonist treatment ameliorates airway hyperreactivity. Nature Communications. 2020;11(1):3998.
https://doi.org/10.1038/s41467-020-17813-1
Haslam A, Prasad V. Estimation of the percentage of US patients with cancer who are eligible for and respond to checkpoint inhibitor immunotherapy drugs. JAMA Network Open. 2019;2(5):e192535–e.
https://doi.org/10.1001/jamanetworkopen.2019.2535
Wang R, Xiong K, Wang Z, Wu D, Hu B, Ruan J, et al. Immunodiagnosis—the promise of personalized immunotherapy. Frontiers in Immunology. 2023;14:1216901.
https://doi.org/10.3389/fimmu.2023.1216901
Okwundu N, Grossman D, Hu-Lieskovan S, Grossmann KF, Swami U. The dark side of immunotherapy. Annals of Translational Medicine. 2021;9(12).
https://doi.org/10.21037/atm-20-4750
Nixon AB, Schalper KA, Jacobs I, Potluri S, Wang I-M, Fleener C. Peripheral immune-based biomarkers in cancer immunotherapy: can we realize their predictive potential? Journal for ImmunoTherapy of Cancer. 2019;7:1–14.
https://doi.org/10.1186/s40425-019-0799-2
Feldmann M, Steinman L. Design of effective immunotherapy for human autoimmunity. Nature. 2005;435(7042):612–9.
https://doi.org/10.1038/nature03727
Jesenak M, Brndiarova M, Urbancikova I, Rennerova Z, Vojtkova J, Bobcakova A, et al. Immune parameters and COVID-19 infection—associations with clinical severity and disease prognosis. Frontiers in Cellular and Infection Microbiology. 2020;10:364.
https://doi.org/10.3389/fcimb.2020.00364
Obeagu EI, Obeagu GU. Utilization of immunological ratios in HIV: implications for monitoring and therapeutic strategies. Medicine. 2024;103(9):e37354.
https://doi.org/10.1097/MD.0000000000037354
Pilard C, Ancion M, Delvenne P, Jerusalem G, Hubert P, Herfs M. Cancer immunotherapy: it's time to better predict patients' response. British Journal of Cancer. 2021;125(7):927–38.
https://doi.org/10.1038/s41416-021-01413-x
Nelde A, Rammensee H-G, Walz JS. The peptide vaccine of the future. Molecular & Cellular Proteomics. 2021;20:100022.
https://doi.org/10.1074/mcp.R120.002309
Fernández VA, Martínez PB, Granhøj JS, Borch TH, Donia M, Svane IM. Biomarkers for response to TIL therapy: a comprehensive review. Journal for ImmunoTherapy of Cancer. 2024;12(3):e008640.
https://doi.org/10.1136/jitc-2023-008640
Catalano M, Iannone LF, Nesi G, Nobili S, Mini E, Roviello G. Immunotherapy-related biomarkers: confirmations and uncertainties. Critical Reviews in Oncology/Hematology. 2023;192:104135.
https://doi.org/10.1016/j.critrevonc.2023.104135
Butterfield LH, Najjar YG. Immunotherapy combination approaches: mechanisms, biomarkers and clinical observations. Nature Reviews Immunology. 2024;24(6):399–416.
https://doi.org/10.1038/s41577-023-00973-8
Miao Y-D, Quan W-X, Tang X-L, Shi W-W, Li Q, Li RJ, et al. Uncovering the flip side of immune checkpoint inhibitors: a comprehensive review of immune-related adverse events and predictive biomarkers. International Journal of Biological Sciences. 2024;20(2):621.
https://doi.org/10.7150/ijbs.89376
Pachner AJ. The brave new world of early treatment of multiple sclerosis: using the molecular biomarkers CXCL13 and neurofilament light to optimize immunotherapy. Biomedicines. 2022;10(9):2099.
https://doi.org/10.3390/biomedicines10092099
Ling SF, Yap CF, Nair N, Bluett J, Morgan AW, Isaacs JD, et al. A proteomics study of rheumatoid arthritis patients on etanercept identifies putative biomarkers associated with clinical outcome measures. Rheumatology. 2024;63(4):1015–21.
https://doi.org/10.1093/rheumatology/kead321
Layhadi JA, Lalioti A, Palmer E, van Zelm MC, Wambre E, Shamji MH, et al. Mechanisms and predictive biomarkers of allergen immunotherapy in the clinic. Journal of Allergy and Clinical Immunology: In Practice. 2024;12(1):59–66.
https://doi.org/10.1016/j.jaip.2023.11.027
Takeuchi T, Miyasaka N, Inui T, Yano T, Yoshinari T, Abe T, et al. High titers of both rheumatoid factor and anti-CCP antibodies at baseline in patients with rheumatoid arthritis are associated with increased circulating baseline TNF level, low drug levels, and reduced clinical responses: a post hoc analysis of the RISING study. Arthritis Research & Therapy. 2017;19:1–11.
https://doi.org/10.1186/s13075-017-1401-2
Harrold LR, Bryson J, Lehman T, Zhuo J, Gao S, Han X, et al. Association between baseline anti-cyclic citrullinated peptide antibodies and 6-month clinical response following abatacept or TNF inhibitor treatment: a real-world analysis of biologic-experienced patients with RA. Rheumatology and Therapy. 2021;8(2):937–53.
https://doi.org/10.1007/s40744-021-00310-2
Julià A, López-Lasanta M, Blanco F, Gómez A, Haro I, Mas AJ, et al. Interactions between rheumatoid arthritis antibodies are associated with the response to anti-tumor necrosis factor therapy. BMC Musculoskeletal Disorders. 2021;22:1–7.
https://doi.org/10.1186/s12891-021-04248-y
Lend K, Lampa J, Padyukov L, Hetland ML, Heiberg MS, Nordström DC, et al. Association of rheumatoid factor, anti-citrullinated protein antibodies and shared epitope with clinical response to initial treatment in patients with early rheumatoid arthritis: data from a randomised controlled trial. Annals of the Rheumatic Diseases. 2024;83(12):1657–65.
https://doi.org/10.1136/ard-2024-226024
Inoue M, Nagafuchi Y, Ota M, Tsuchiya H, Tateishi S, Kanda H, et al. Carriers of HLA-DRB1*04:05 have a better clinical response to abatacept in rheumatoid arthritis. Scientific Reports. 2023;13(1):15250.
https://doi.org/10.1038/s41598-023-42324-6
Cha S, Bang S-Y, Joo YB, Cho S-K, Choi C-B, Sung Y-K, et al. Association of HLA-DRB1 locus with treatment response to abatacept or TNF inhibitors in patients with seropositive rheumatoid arthritis. Scientific Reports. 2024;14(1):6763.
https://doi.org/10.1038/s41598-024-56987-2
Delcoigne B, Manouchehrinia A, Barro C, Benkert P, Michalak Z, Kappos L, et al. Blood neurofilament light levels segregate treatment effects in multiple sclerosis. Neurology. 2020;94(11):e1201–12.
https://doi.org/10.1212/WNL.0000000000009097
Sormani MP, Haering DA, Kropshofer H, Leppert D, Kundu U, Barro C, et al. Blood neurofilament light as a potential endpoint in phase 2 studies in MS. Annals of Clinical and Translational Neurology. 2019;6(6):1081–9.
https://doi.org/10.1002/acn3.795
Dalla Costa G, Martinelli V, Moiola L, Sangalli F, Colombo B, Finardi A, et al. Serum neurofilaments increase at progressive multifocal leukoencephalopathy onset in natalizumab‐treated multiple sclerosis patients. Annals of Neurology. 2019;85(4):606–10.
https://doi.org/10.1002/ana.25437
Fissolo N, Pignolet B, Rio J, Vermersch P, Ruet A, Desèze J, et al. Serum neurofilament levels and PML risk in patients with multiple sclerosis treated with natalizumab. Neurology: Neuroimmunology & Neuroinflammation. 2021;8(4):e1003.
https://doi.org/10.1212/NXI.0000000000001003
Abdelhak A, Antweiler K, Kowarik MC, Senel M, Havla J, Zettl UK, et al. Serum glial fibrillary acidic protein and disability progression in progressive multiple sclerosis. Annals of Clinical and Translational Neurology. 2024;11(2):477–85.
https://doi.org/10.1002/acn3.51969
Talaat F, Abdelatty S, Ragaie C, Dahshan A. Chitinase-3-like 1 protein in CSF: a novel biomarker for progression in patients with multiple sclerosis. Neurological Sciences. 2023;44(9):3243–52.
https://doi.org/10.1007/s10072-023-06764-2
Bordas‐Le Floch V, Berjont N, Batard T, Varese N, O'Hehir RE, Canonica WG, et al. Coordinated IgG2 and IgE responses as a marker of allergen immunotherapy efficacy. Allergy. 2022;77(4):1263–73.
https://doi.org/10.1111/all.15107
Ortega HG, Yancey SW, Mayer B, Gunsoy NB, Keene ON, Bleecker ER, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. The Lancet Respiratory Medicine. 2016;4(7):549–56.
https://doi.org/10.1016/S2213-2600(16)30031-5
Celis-Preciado CA, Lachapelle P, Couillard S. Blood eosinophils take centre stage in predicting the response to sublingual immunotherapy (SLIT): a familiar twist. Thorax. 2024;79(5):297–8.
https://doi.org/10.1136/thorax-2023-221274
Katz LE, Gleich GJ, Hartley BF, Yancey SW, Ortega HG. Blood eosinophil count is a useful biomarker to identify patients with severe eosinophilic asthma. Annals of the American Thoracic Society. 2014;11(4):531–6.
https://doi.org/10.1513/AnnalsATS.201310-354OC
Ogulur I, Pat Y, Ardicli O, Barletta E, Cevhertas L, Fernandez‐Santamaria R, et al. Advances and highlights in biomarkers of allergic diseases. Allergy. 2021;76(12):3659–86.
https://doi.org/10.1111/all.15089
Pavord ID, Deniz Y, Corren J, Casale TB, FitzGerald JM, Izuhara K, et al. Baseline FeNO independently predicts the dupilumab response in patients with moderate-to-severe asthma. Journal of Allergy and Clinical Immunology: In Practice. 2023;11(4):1213–20.e2.
https://doi.org/10.1016/j.jaip.2022.11.043
Hoshino M, Akitsu K, Kubota K, Ohtawa J. Association between biomarkers and house dust mite sublingual immunotherapy in allergic asthma. Clinical and Experimental Allergy. 2020;50(9):1035–43.
https://doi.org/10.1111/cea.13686
Li T, Li Y, Zhu X, He Y, Wu Y, Ying T, et al., editors. Artificial intelligence in cancer immunotherapy: applications in neoantigen recognition, antibody design and immunotherapy response prediction. Seminars in Cancer Biology. 2023.
Li Y, Wu X, Fang D, Luo Y. Informing immunotherapy with multi-omics driven machine learning. npj Digital Medicine. 2024;7(1):67.
https://doi.org/10.1038/s41746-024-01043-6
Peng J, Zhang J, Zou D, Xiao L, Ma H, Zhang X, et al. Deep learning to estimate durable clinical benefit and prognosis from patients with non-small cell lung cancer treated with PD-1/PD-L1 blockade. Frontiers in Immunology. 2022;13:960459.
https://doi.org/10.3389/fimmu.2022.960459
Wang Y, Chen L, Ju L, Xiao Y, Wang X. Tumor mutational burden related classifier is predictive of response to PD-L1 blockade in locally advanced and metastatic urothelial carcinoma. International Immunopharmacology. 2020;87:106818.
https://doi.org/10.1016/j.intimp.2020.106818
Liu R, Dollinger E, Nie Q. Machine learning of single cell transcriptomic data from anti-PD-1 responders and non-responders reveals distinct resistance mechanisms in skin cancers and PDAC. Frontiers in Genetics. 2022;12:806457.
https://doi.org/10.3389/fgene.2021.806457
Kang Y, Vijay S, Gujral TS. Deep neural network modeling identifies biomarkers of response to immune-checkpoint therapy. iScience. 2022;25(5):104228.
https://doi.org/10.1016/j.isci.2022.104228
Sidhom J-W, Ross-Macdonald P, Wind-Rotolo M, Pardoll A, Baras A. Deep learning reveals predictive sequence concepts within immune repertoires to immunotherapy. Journal for ImmunoTherapy of Cancer. 2021;9(Suppl):A832.
https://doi.org/10.1136/jitc-2021-SITC2021.832
Yoo S-K, Fitzgerald CW, Cho BA, Fitzgerald BG, Han C, Koh ES, et al. Prediction of checkpoint inhibitor immunotherapy efficacy for cancer using routine blood tests and clinical data. 2025:1–12.
Li X, Dowling EK, Yan G, Dereli Z, Bozorgui B, Imanirad P, et al. Precision combination therapies based on recurrent oncogenic coalterations. Cancer Discovery. 2022;12(6):1542–59.
https://doi.org/10.1158/2159-8290.CD-21-0832
Yin J, Xu L, Wang S, Zhang L, Zhang Y, Zhai Z, et al. Integrating immune multi-omics and machine learning to improve prognosis, immune landscape, and sensitivity to first- and second-line treatments for head and neck squamous cell carcinoma. Scientific Reports. 2024;14(1):31454.
https://doi.org/10.1038/s41598-024-83184-y
Gschwind A, Ossowski S. AI model for predicting anti-PD1 response in melanoma using multi-omics biomarkers. Cancers. 2025;17(5):714.
https://doi.org/10.3390/cancers17050714
Tao W, Concepcion AN, Vianen M, Marijnissen AC, Lafeber FP, Radstake TR, et al. Multiomics and machine learning accurately predict clinical response to adalimumab and etanercept therapy in patients with rheumatoid arthritis. Arthritis & Rheumatology. 2021;73(2):212–22.
https://doi.org/10.1002/art.41516
Edner NM, Heuts F, Thomas N, Wang CJ, Petersone L, Kenefeck R, et al. Follicular helper T cell profiles predict response to costimulation blockade in type 1 diabetes. Nature Immunology. 2020;21(10):1244–55.
https://doi.org/10.1038/s41590-020-0744-z
Wang D, Lv Q, Yao H, Chen Y, Yu J, Jin X, et al. The efficacy prediction of subcutaneous immunotherapy for pediatric allergic rhinitis: application of machine learning methods. Biomedical Signal Processing and Control. 2026;112:108704.
https://doi.org/10.1016/j.bspc.2025.108704
Yao H, Wang L, Zhou X, Jia X, Xiang Q, Zhang W, et al. Predicting the therapeutic efficacy of AIT for asthma using clinical characteristics, serum allergen detection metrics, and machine learning techniques. Computers in Biology and Medicine. 2023;166:107544.
https://doi.org/10.1016/j.compbiomed.2023.107544
Salehi F, Zarifi S, Bayat S, Habibpour M, Asemanrafat A, Kleyer A, et al. Predicting Disease Activity Score in rheumatoid arthritis patients treated with biologic disease-modifying antirheumatic drugs using machine learning models. Technologies. 2025;13(8):350.
https://doi.org/10.3390/technologies13080350
Suárez-Fariñas M, Suprun M, Chang HL, Gimenez G, Grishina G, Getts R, et al. Predicting development of sustained unresponsiveness to milk oral immunotherapy using epitope-specific antibody binding profiles. Journal of Allergy and Clinical Immunology. 2019;143(3):1038–46.
https://doi.org/10.1016/j.jaci.2018.10.028
Liu R, Rizzo S, Wang L, Chaudhary N, Maund S, Garmhausen MR, et al. Characterizing mutation-treatment effects using clinico-genomics data of 78,287 patients with 20 types of cancers. Nature Communications. 2024;15(1):10884.
https://doi.org/10.1038/s41467-024-55251-5
Jee J, Fong C, Pichotta K, Tran TN, Luthra A, Waters M, et al. Automated real-world data integration improves cancer outcome prediction. 2024:1–9.
Yang Y, Yang J, Shen L, Chen J, Xia L, Ni B, et al. A multi-omics-based serial deep learning approach to predict clinical outcomes of single-agent anti-PD-1/PD-L1 immunotherapy in advanced stage non-small-cell lung cancer. 2021;13(2):743.
Wang N, Song J, Sun SR, Zhu KZ, Li JX, Wang ZC, et al. Immune signatures predict response to house dust mite subcutaneous immunotherapy in patients with allergic rhinitis. Allergy. 2024;79(5):1230–41.
https://doi.org/10.1111/all.16068
Ferrè L, Clarelli F, Pignolet B, Mascia E, Frasca M, Santoro S, et al. Combining clinical and genetic data to predict response to fingolimod treatment in relapsing remitting multiple sclerosis patients: a precision medicine approach. Journal of Personalized Medicine. 2023;13(1):122.
https://doi.org/10.3390/jpm13010122
Bouget V, Duquesne J, Hassler S, Cournède P-H, Fautrel B, Guillemin F, et al. Machine learning predicts response to TNF inhibitors in rheumatoid arthritis: results on the ESPOIR and ABIRISK cohorts. RMD Open. 2022;8(2):e002442.
https://doi.org/10.1136/rmdopen-2022-002442
Zhou Z, Wang J, Wang J, Yang S, Wang R, Zhang G, et al. Deciphering the tumor immune microenvironment from a multidimensional omics perspective: insight into next-generation CAR-T cell immunotherapy and beyond. Molecular Cancer. 2024;23(1):131.
https://doi.org/10.1186/s12943-024-02047-2
MacMath D, Chen M, Khoury P. Artificial intelligence: exploring the future of innovation in allergy immunology. Current Allergy and Asthma Reports. 2023;23(6):351–62.
https://doi.org/10.1007/s11882-023-01084-z
Yoosuf N, Maciejewski M, Ziemek D, Jelinsky SA, Folkersen L, Müller M, et al. Early prediction of clinical response to anti-TNF treatment using multi-omics and machine learning in rheumatoid arthritis. Rheumatology. 2022;61(4):1680–9.
https://doi.org/10.1093/rheumatology/keab521
Fousteri G, Rodrigues EM, Giamporcaro GM, Falcone M. A machine learning approach to predict response to immunotherapy in type 1 diabetes. Cellular & Molecular Immunology. 2021;18(3):515–7.
https://doi.org/10.1038/s41423-020-00594-4
Gautier T, Ziegler LB, Gerber MS, Campos-Náñez E, Patek SD. Artificial intelligence and diabetes technology: a review. Metabolism. 2021;124:154872.
https://doi.org/10.1016/j.metabol.2021.154872
Chitnis T, Prat A. A roadmap to precision medicine for multiple sclerosis. Multiple Sclerosis Journal. 2020;26(5):522–32.
https://doi.org/10.1177/1352458519881558
Engel S, Zipp F. Preventing disease progression in multiple sclerosis—insights from large real-world cohorts. Genome Medicine. 2022;14(1):41.
https://doi.org/10.1186/s13073-022-01044-8
Engelhardt B, Comabella M, Chan A. Multiple sclerosis: immunopathological heterogeneity and its implications. European Journal of Immunology. 2022;52(6):869–81.
https://doi.org/10.1002/eji.202149757
Masina R, Caldas C. Precision cancer medicine 2.0—oncology in the postgenomic era. Molecular Oncology. 2024;18(9):2065–9.
https://doi.org/10.1002/1878-0261.13707
Celi LA, Cellini J, Charpignon M-L, Dee EC, Dernoncourt F, Eber R, et al. Sources of bias in artificial intelligence that perpetuate healthcare disparities—a global review. PLOS Digital Health. 2022;1(3):e0000022.
https://doi.org/10.1371/journal.pdig.0000022
Zou J, Schiebinger L. AI can be sexist and racist—it's time to make it fair. Nature. 2018;559:324–6.
https://doi.org/10.1038/d41586-018-05707-8
Wang J, Zeng Z, Li Z, Liu G, Zhang S, Luo C, et al. The clinical application of artificial intelligence in cancer precision treatment. Journal of Translational Medicine. 2025;23(1):120.
https://doi.org/10.1186/s12967-025-06139-5
Wadden JJ. Defining the undefinable: the black box problem in healthcare artificial intelligence. Journal of Medical Ethics. 2022;48(10):764–8.
https://doi.org/10.1136/medethics-2021-107529
Gerlings J, Jensen MS, Shollo A. Explainable AI, but explainable to whom? An exploratory case study of xAI in healthcare. In: Handbook of Artificial Intelligence in Healthcare. Vol 2: Practicalities and Prospects. Springer; 2021. p. 169–98.
https://doi.org/10.1007/978-3-030-83620-7_7
Palaniappan K, Lin EYT, Vogel S, editors. Global regulatory frameworks for the use of artificial intelligence (AI) in the healthcare services sector. Healthcare. 2024;12(5):562.
https://doi.org/10.3390/healthcare12050562
Van Kolfschooten H, Van Oirschot J. The EU Artificial Intelligence Act (2024): implications for healthcare. Health Policy. 2024;149:105152.
https://doi.org/10.1016/j.healthpol.2024.105152
Han L, Chen Y, Wang L, Zong X. Discussion on the regulatory test of artificial intelligence-enabled medical devices and their technical potential in tumor immunity. Technology in Cancer Research & Treatment. 2025;24(3):1–14.
https://doi.org/10.54963/ti.v9i3.1217
Yang C, Chen Y, Qian C, Shi F, Guo Y. The data-intensive research paradigm: challenges and responses in clinical professional graduate education. Frontiers in Medicine. 2025;12:1461863.
https://doi.org/10.3389/fmed.2025.1461863
Maliha G, Gerke S, Cohen IG, Parikh RB. Artificial intelligence and liability in medicine: balancing safety and innovation. Milbank Quarterly. 2021;99(3):629–67.
https://doi.org/10.1111/1468-0009.12504
Pachner AR, Pike SC, Smith AD, Gilli F. The CXCL13 index biomarker predicts success or failure of moderate-efficacy disease-modifying therapies in multiple sclerosis: a real-world study. Multiple Sclerosis and Related Disorders. 2025;95:106303.
https://doi.org/10.1016/j.msard.2025.106303
Assis A, Dantas J, Andrade E. The performance–interpretability trade-off: a comparative study of machine learning models. Journal of Reliable Intelligent Environments. 2025;11(1):1–14.
https://doi.org/10.1007/s40860-024-00240-0
Abdullah TA, Zahid MSM, Ali W. A review of interpretable ML in healthcare: taxonomy, applications, challenges, and future directions. Symmetry. 2021;13(12):2439.
https://doi.org/10.3390/sym13122439
Prelaj A, Galli EG, Miskovic V, Pesenti M, Viscardi G, Pedica B, et al. Real-world data to build explainable trustworthy artificial intelligence models for prediction of immunotherapy efficacy in NSCLC patients. Frontiers in Oncology. 2023;12:1078822.
https://doi.org/10.3389/fonc.2022.1078822
Hounye AH, Xiong L, Hou M. Integrated explainable machine learning and multi-omics analysis for survival prediction in cancer with immunotherapy response. Apoptosis. 2025;30(1):364–88.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2026 Ritika Sharma

This work is licensed under a Creative Commons Attribution 4.0 International License.









