Complementary therapies in early breast cancer: Oncologists’ evidence-based decisions in a Southeast European vignette survey
DOI:
https://doi.org/10.17305/bb.2025.13413Keywords:
Integrative medicine, integrative oncology, breast neoplasms, complementary therapiesAbstract
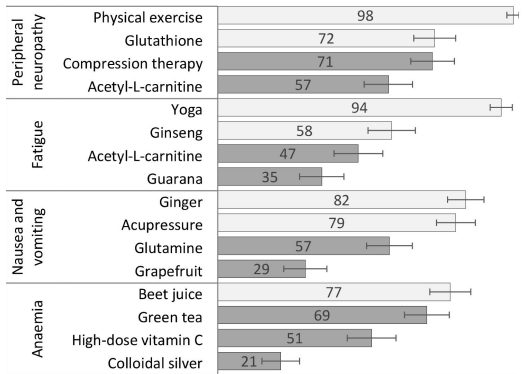
Complementary therapies are increasingly integrated into the framework of integrative oncology. While numerous complementary therapies provide potential benefits, some may also carry risks, including interactions with conventional cancer treatments. The degree to which oncologists' real-world decisions regarding complementary therapies align with evidence-based guidelines remains uncertain. This study aimed to evaluate oncologists' evidence-based decisions on whether specific complementary therapies should be prohibited, permitted, or recommended for early breast cancer treatment. We conducted a cross-sectional online survey that included a randomized vignette experiment involving oncology specialists and residents from seven Southeast European countries. The primary outcome was the percentage of accurate classifications of 28 therapy-indication pairs in neoadjuvant and adjuvant settings, benchmarked against published evidence. Correctness was assessed using both a strict definition (one correct option) and an expanded definition (accepting "allow" or "recommend" when supported by evidence). A total of 136 respondents met the inclusion criteria and provided paired responses. Median accuracy was found to be 52% (95% CI 48-55) under the strict definition and 70% (95% CI 67-72) under the expanded definition, with no significant differences observed between neoadjuvant and adjuvant settings. Evidence-based therapies, such as physical exercise and cognitive behavioral therapy, were most frequently recommended, whereas most other therapies received endorsement from fewer than 25% of respondents. Overall, oncologists exhibited moderate alignment with evidence, demonstrating a tendency to permit rather than actively recommend complementary therapies, even when evidence indicated potential benefits and safety. These findings underscore the necessity for targeted educational interventions aimed at enhancing oncologists' understanding and ensuring the safe and informed integration of complementary therapies into clinical practice.
Citations
Downloads
References
National Cancer Institute. Complementary and Alternative Medicine (CAM) [Internet]. National Cancer Institute; [cited 2025 Jun 30]. Available from: https://www.cancer.gov/about-cancer/treatment/cam
Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012;11(3):187–203.
https://doi.org/10.1177/1534735411423920
Molassiotis A, Fernadez-Ortega P, Pud D, Ozden G, Scott JA, Panteli V, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16(4):655–63.
https://doi.org/10.1093/annonc/mdi110
Jazieh AR, Abuelgasim KA, Ardah HI, Alkaiyat M, Da'ar OB. The trends of complementary alternative medicine use among cancer patients. BMC Complement Med Ther. 2021;21(1):167.
https://doi.org/10.1186/s12906-021-03338-7
Greenlee H, DuPont-Reyes MJ, Balneaves LG, Carlson LE, Cohen MR, Deng G, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J Clin. 2017;67(3):194–232.
https://doi.org/10.3322/caac.21397
Witt CM, Cardoso MJ. Complementary and integrative medicine for breast cancer patients – Evidence based practical recommendations. Breast. 2016;28:37–44.
https://doi.org/10.1016/j.breast.2016.04.012
Yun H, Sun L, Mao JJ. Growth of integrative medicine at leading cancer centers between 2009 and 2016: a systematic analysis of NCI-designated comprehensive cancer center websites. JNCI Monogr. 2017;2017(52):lgx004.
https://doi.org/10.1093/jncimonographs/lgx004
World Health Organization, Programme on Traditional Medicine. WHO traditional medicine strategy 2002–2005. Geneva: World Health Organization; 2002.
https://apps.who.int/iris/handle/10665/67163. Accessed 15 Feb 2023.
Wode K, Henriksson R, Sharp L, Stoltenberg A, Hök Nordberg J. Cancer patients' use of complementary and alternative medicine in Sweden: a cross-sectional study. BMC Complement Altern Med. 2019;19(1):62.
https://doi.org/10.1186/s12906-019-2452-5
Mathijssen RHJ, Verweij J, de Bruijn P, Loos WJ, Sparreboom A. Effects of St. John's wort on irinotecan metabolism. J Natl Cancer Inst. 2002;94(16):1247–9.
https://doi.org/10.1093/jnci/94.16.1247
Golden EB, Lam PY, Kardosh A, Gaffney KJ, Cadenas E, Louie SG, et al. Green tea polyphenols block the anticancer effects of bortezomib and other boronic acid-based proteasome inhibitors. Blood. 2009;113(23):5927–37.
https://doi.org/10.1182/blood-2008-07-171389
Heaney ML, Gardner JR, Karasavvas N, Golde DW, Scheinberg DA, Smith EA, et al. Vitamin C antagonizes the cytotoxic effects of antineoplastic drugs. Cancer Res. 2008;68(19):8031–8.
https://doi.org/10.1158/0008-5472.CAN-08-1490
Loq uai C, Dechent D, Garzarolli M, Kaatz M, Kaehler KC, Kurschat P, et al. Risk of interactions between complementary and alternative medicine and medication for comorbidities in patients with melanoma. Med Oncol. 2016;33(5):52.
https://doi.org/10.1007/s12032-016-0764-6
Dong B, Xie C, Jing X, Lin L, Tian L. Yoga has a solid effect on cancer-related fatigue in patients with breast cancer: a meta-analysis. Breast Cancer Res Treat. 2019;177(1):5–16.
https://doi.org/10.1007/s10549-019-05278-w
Wayne PM, Lee MS, Novakowski J, Osypiuk K, Ligibel J, Carlson LE, et al. Tai Chi and Qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv. 2018;12(2):256–67.
https://doi.org/10.1007/s11764-017-0665-5
Molassiotis A, Helin AM, Dabbour R, Hummerston S. The effects of P6 acupressure in the prophylaxis of chemotherapy-related nausea and vomiting in breast cancer patients. Complement Ther Med. 2007;15(1):3–12.
https://doi.org/10.1016/j.ctim.2006.07.005
Listing M, Reißhauer A, Krohn M, Voigt B, Tjahono G, Becker J, et al. Massage therapy reduces physical discomfort and improves mood disturbances in women with breast cancer. Psychooncology. 2009;18(12):1290–9.
https://doi.org/10.1002/pon.1508
Henderson VP, Clemow L, Massion AO, Hurley TG, Druker S, Hébert JR. The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Res Treat. 2012;131(1):99–109.
https://doi.org/10.1007/s10549-011-1738-1
Key TJ, Bradbury KE, Perez-Cornago A, Sinha R, Tsilidis KK, Tsugane S. Diet, nutrition, and cancer risk: what do we know and what is the way forward? BMJ. 2020;368:m511.
https://doi.org/10.1136/bmj.m511
McTiernan A, Friedenreich CM, Katzmarzyk PT, Powell KE, Macko R, Buchner D, et al. Physical activity in cancer prevention and survival: a systematic review. Med Sci Sports Exerc. 2019;51(6):1252–61.
https://doi.org/10.1249/MSS.0000000000001937
Courneya KS, Vardy JL, O'Callaghan CJ, Gill S, Friedenreich CM, Wong RKS, et al. Structured exercise after adjuvant chemotherapy for colon cancer. N Engl J Med. 2025;393(1):13–25.
https://doi.org/10.1056/NEJMoa2502760
King N, Balneaves LG, Levin GT, Nguyen T, Nation JG, Card C, et al. Surveys of cancer patients and cancer health care providers regarding complementary therapy use, communication, and information needs. Integr Cancer Ther. 2015;14(6):515–24.
https://doi.org/10.1177/1534735415589984
Smithson J, Paterson C, Britten N, Evans M, Lewith G. Cancer patients' experiences of using complementary therapies: polarization and integration. J Health Serv Res Policy. 2010;15 Suppl 2:54–61.
https://doi.org/10.1258/jhsrp.2009.009104
Stub T, Quandt SA, Arcury TA, Sandberg JC, Kristoffersen AE, Musial F, et al. Perception of risk and communication among conventional and complementary health care providers involving cancer patients' use of complementary therapies: a literature review. BMC Complement Altern Med. 2016;16(1):353.
https://doi.org/10.1186/s12906-016-1326-3
Maha N, Shaw A. Academic doctors' views of complementary and alternative medicine (CAM) and its role within the NHS: an exploratory qualitative study. BMC Complement Altern Med. 2007;7:17.
https://doi.org/10.1186/1472-6882-7-17
Saha S, Beach MC. The impact of patient-centered communication on patients' decision making and evaluations of physicians: a randomized study using video vignettes. Patient Educ Couns. 2011;84(3):386–92.
https://doi.org/10.1016/j.pec.2011.04.023
Johnston SRD, Toi M, O'Shaughnessy J, Rastogi P, Campone M, Neven P, et al. Abemaciclib plus endocrine therapy for hormone receptor-positive, HER2-negative, node-positive, high-risk early breast cancer (monarchE): results from a preplanned interim analysis of a randomised, open-label, phase 3 trial. Lancet Oncol. 2023;24(1):77–90.
https://doi.org/10.1016/S1470-2045(22)00694-5
Geyer CE, Garber JE, Gelber RD, Yothers G, Taboada M, Ross L, et al. Overall survival in the OlympiA phase III trial of adjuvant olaparib in patients with germline pathogenic variants in BRCA1/2 and high-risk, early breast cancer. Ann Oncol. 2022;33(12):1250–68.
https://doi.org/10.1016/j.annonc.2022.09.159
Schipilliti FM, Drittone D, Mazzuca F, La Forgia D, Guven DC, Rizzo A. Datopotamab deruxtecan: a novel antibody drug conjugate for triple-negative breast cancer. Heliyon. 2024;10(7):e28385.
https://doi.org/10.1016/j.heliyon.2024.e28385
Caputo R, Buono G, Piezzo M, Martinelli C, Cianniello D, Rizzo A, et al. Sacituzumab govitecan for the treatment of advanced triple negative breast cancer patients: a multi-center real-world analysis. Front Oncol. 2024;14:1362641.
https://doi.org/10.3389/fonc.2024.1362641
Bower JE, Lacchetti C, Alici Y, Barton DL, Bruner D, Canin BE, et al. Management of fatigue in adult survivors of cancer: ASCO-Society for Integrative Oncology guideline update. J Clin Oncol. 2024;42(20):2456–87.
https://doi.org/10.1200/JCO.24.00541
Carlson LE, Ismaila N, Addington EL, Asher GN, Atreya C, Balneaves LG, et al. Integrative oncology care of symptoms of anxiety and depression in adults with cancer: Society for Integrative Oncology-ASCO guideline. J Clin Oncol. 2023;41(28):4562–91.
https://doi.org/10.1200/JCO.23.00857
National Comprehensive Cancer Network. Cancer-related fatigue. Version 1.2026 [Internet]. 2025 Nov. Available from: https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf
Loprinzi CL, Lacchetti C, Bleeker J, Cavaletti G, Chauhan C, Hertz DL, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: ASCO guideline update. J Clin Oncol. 2020;38(28):3325–48.
https://doi.org/10.1200/JCO.20.01399
Fasinu PS, Rapp GK. Herbal interaction with chemotherapeutic drugs – a focus on clinically significant findings. Front Oncol. 2019;9:1356.
https://doi.org/10.3389/fonc.2019.01356
Over-the-counter drug products containing colloidal silver ingredients or silver salts. Department of Health and Human Services (HHS), Public Health Service (PHS), Food and Drug Administration (FDA). Final rule. Fed Regist. 1999;64(158):44653–8.
Zeller T, Muenstedt K, Stoll C, Schweder J, Senf B, Ruckhaeberle E, et al. Potential interactions of complementary and alternative medicine with cancer therapy in outpatients with gynecological cancer in a comprehensive cancer center. J Cancer Res Clin Oncol. 2013;139(3):357–65.
https://doi.org/10.1007/s00432-012-1336-6
Acosta L, Byham-Gray L, Kurzer M, Samavat H. Hepatotoxicity with high-dose green tea extract: effect of catechol-O-methyltransferase and uridine 5'-diphospho-glucuronosyltransferase 1A4 genotypes. J Diet Suppl. 2023;20(6):850–69.
https://doi.org/10.1080/19390211.2022.2128501
Ma Y, Hall DL, Ngo LH, Liu Q, Bain PA, Yeh GY. Efficacy of cognitive behavioural therapy for insomnia in breast cancer: a meta-analysis. Sleep Med Rev. 2021;55:101376.
https://doi.org/10.1016/j.smrv.2020.101376
Seo K, Kim JH, Han D. Effects of melatonin supplementation on sleep quality in breast cancer patients: a systematic review and meta-analysis. Healthcare (Basel). 2023;11(5):675.
https://doi.org/10.3390/healthcare11050675
Sovak M, Seligson AL, Konas M, Hajduch M, Dolezal M, Machala M, et al. Herbal composition PC-SPES for management of prostate cancer: identification of active principles. J Natl Cancer Inst. 2002;94(17):1275–81.
https://doi.org/10.1093/jnci/94.17.1275
Mei N, Guo L, Fu PP, Fuscoe JC, Luan Y, Chen T. Metabolism, genotoxicity, and carcinogenicity of comfrey. J Toxicol Environ Health Crit Rev. 2010;13(7–8):509–26.
https://doi.org/10.1080/10937404.2010.509013
Brown AC. Liver toxicity related to herbs and dietary supplements: online table of case reports. Part 2 of 5 series. Food Chem Toxicol. 2017;107:472–501.
https://doi.org/10.1016/j.fct.2016.07.001
Bonett DG, Price RM. Statistical inference for a linear function of medians: confidence intervals, hypothesis testing, and sample size requirements. Psychol Methods. 2002;7(3):370–83.
https://doi.org/10.1037/1082-989X.7.3.370
Vrdoljak E, Bodoky G, Jassem J, Popescu RA, Mardiak J, Pirker R, et al. Cancer control in Central and Eastern Europe: current situation and recommendations for improvement. The Oncologist. 2016;21(10):1183–90.
https://doi.org/10.1634/theoncologist.2016-0137
Smithson M, Verkuilen J. A better lemon squeezer? Maximum-likelihood regression with beta-distributed dependent variables. Psychol Methods. 2006;11(1):54–71.
https://doi.org/10.1037/1082-989X.11.1.54
Chang KH, Brodie R, Choong MA, Sweeney KJ, Kerin MJ. Complementary and alternative medicine use in oncology: a questionnaire survey of patients and health care professionals. BMC Cancer. 2011;11:196.
https://doi.org/10.1186/1471-2407-11-196
Al-Omari A, Al-Qudimat M, Abu Hmaidan A, Zaru L. Perception and attitude of Jordanian physicians towards complementary and alternative medicine (CAM) use in oncology. Complement Ther Clin Pract. 2013;19(2):70–6.
https://doi.org/10.1016/j.ctcp.2013.01.002
Berretta M, Rinaldi L, Taibi R, Tralongo P, Fulvi A, Montesarchio V, et al. Physician attitudes and perceptions of complementary and alternative medicine (CAM): a multicentre Italian study. Front Oncol. 2020;10:594.
https://doi.org/10.3389/fonc.2020.00594
Lee RT, Barbo A, Lopez G, Melhem-Bertrandt A, Lin H, Olopade OI, et al. National survey of US oncologists' knowledge, attitudes, and practice patterns regarding herb and supplement use by patients with cancer. J Clin Oncol. 2014;32(36):4095–101.
https://doi.org/10.1200/JCO.2014.55.8676
Yang G, Lee R, Zhang H, Gu W, Yang P, Ling C. National survey of China's oncologists' knowledge, attitudes, and clinical practice patterns on complementary and alternative medicine. Oncotarget. 2017;8(8):13440–9.
https://doi.org/10.18632/oncotarget.14560
De Azambuja E, Ameye L, Paesmans M, Zielinski CC, Piccart-Gebhart M, Preusser M. The landscape of medical oncology in Europe by 2020. Ann Oncol. 2014;25(2):525–8.
https://doi.org/10.1093/annonc/mdt559
Mathew A. Global survey of clinical oncology workforce. J Glob Oncol. 2018;(4):1–12.
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2025 Teo Buhovac, Žarko Bajić, Mario Nalbani, Lazar Popović, Milan Risteski, Nikola Milašević, George Dimitrov, Anes Pašić, Marija Karaga, Eduard Vrdoljak

This work is licensed under a Creative Commons Attribution 4.0 International License.









