Changes in inflammatory responses and autophagy during apheresis platelet preservation and their correlation with platelet transfusion refractoriness in patients with acute lymphoblastic leukemia
DOI:
https://doi.org/10.17305/bb.2023.9216Keywords:
Apheresis platelets (APs), platelet transfusion, platelet transfusion refractoriness (PTR), acute lymphoblastic leukemia (ALL), inflammatory response, autophagy, platelet preservation, peripheral blood mononuclear cells (PBMCs)Abstract
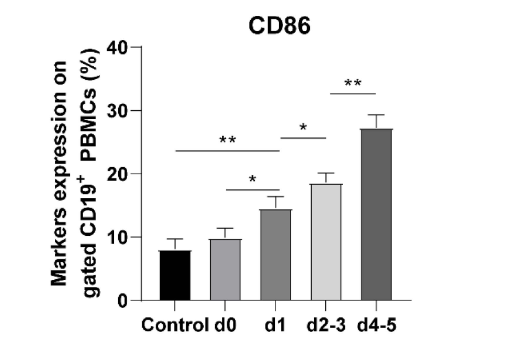
Acute lymphoblastic leukemia (ALL) is a common hematopoietic malignancy, and platelet transfusion plays a crucial role in its treatment. This study aimed to investigate the changes in inflammatory response and autophagy during the preservation of apheresis platelets (AP) and their correlation with platelet transfusion refractoriness (PTR) in ALL. ALL patients were included, and APs were categorized based on the preservation period (day 0, day 1, days 2-3, and days 4-5). The activation factors procaspase-activating compound 1 (PAC-1) and P-selectin (CD62P), AP aggregation function, inflammation levels (interleukin 1 beta [IL-1β], interleukin 6 [IL-6], tumor necrosis factor alpha [TNF-α] and NOD-like receptor thermal protein domain associated protein 3 [NLRP3]), and autophagy-related genes (p62) during AP preservation were assessed. Following co-culturing APs with peripheral blood mononuclear cells (PBMCs), specific activation markers were studied to observe APs influence on immune cells activation. The effectiveness of platelet transfusion was assessed, and risk factors for PTR were analyzed. As the storage duration of AP increased, the activation factors, coagulation factor activity, inflammation levels, and the activation of immune cells in AP increased, while fibrinogen levels and AP aggregation function decreased. The expression levels of autophagy-related genes (the autophagy marker light chain 3B gene [LC3B] and Beclin 1 gene) decreased with prolongation preservation. The effective rate of AP transfusion in ALL patients was 68.21%. AP preservation time, IL-6, p62, and Beclin 1 were identified as independent risk factors affecting PTR in ALL patients. In conclusion, during AP preservation, inflammation, autophagy, and activation of immune cells were observed to increase. AP preservation time, IL-6, p62, and Beclin 1 were independent risk factors for PTR.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2023 Ying Li, Zhiqun Song, Xiaohong Sun, Juanjuan Tang, Xiaoyu Zhou

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2023-06-20
Published 2023-11-03









