Sugammadex vs neostigmine in post-anesthesia recovery: A systematic review and meta-analysis
DOI:
https://doi.org/10.17305/bb.2025.12689Keywords:
Sugammadex, neostigmine, recovery, TOF, PONV, PPCs, cognitive functionAbstract
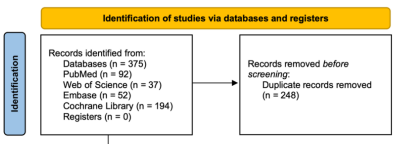
Residual neuromuscular blockade (RNB) is linked to an increased risk of perioperative adverse events. This study systematically evaluates the impact of neuromuscular blockade antagonists on postoperative complications and quality of recovery in surgical patients. We conducted a systematic review and meta-analysis to compare the efficacy of sugammadex and neostigmine. Comprehensive searches were performed across medical databases, including Web of Science, PubMed, Embase, and the Cochrane Library, with a final search date of April 6, 2025. A total of thirty-five randomized controlled trials (RCTs) involving 4,275 patients, along with two retrospective studies comprising 49,642 participants, met the inclusion criteria. The meta-analysis revealed that sugammadex facilitated faster reversal of RNB compared to neostigmine, as indicated by a quicker recovery to a train-of-four ratio (TOFR) ≥ 0.9 (standardized mean difference [SMD] -3.45; 95% confidence interval [CI], -4.42 to -2.48), a shorter extubation time (SMD -1.44; 95% CI, -2.02 to -0.85), and a decreased incidence of RNB (risk ratio [RR] 0.18; 95% CI, 0.07 to 0.47). Moreover, sugammadex significantly reduced postoperative complications compared to neostigmine, including the incidence of postoperative nausea and vomiting (PONV) (RR 0.64; 95% CI, 0.46 to 0.88), postoperative pulmonary complications (PPCs) (RR 0.62; 95% CI, 0.38 to 0.99), and bradycardia (RR 0.32; 95% CI, 0.20 to 0.50). In conclusion, sugammadex provides a faster reversal of neuromuscular blockade compared to neostigmine and is associated with a reduction in postoperative complications. However, this expedited reversal does not result in measurable improvements in overall recovery quality, nor do either sugammadex or neostigmine significantly affect postoperative cognitive function.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2025 Ni Zhu, Yongli Li

This work is licensed under a Creative Commons Attribution 4.0 International License.









