HbA1c variability and risk of incident heart failure: A systematic review and meta-analysis
DOI:
https://doi.org/10.17305/bb.2025.13376Keywords:
Glycated hemoglobin, variability, heart failure, risk factor, meta-analysisAbstract
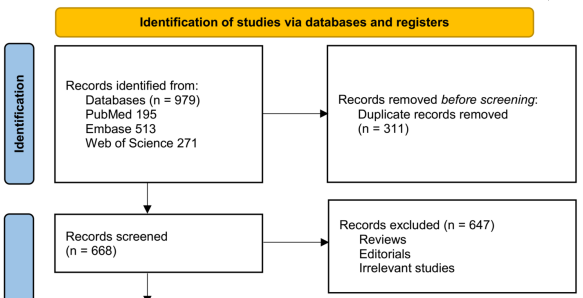
Visit-to-visit variability in glycated hemoglobin (HbA1c) reflects long-term instability in glycemic control, potentially contributing to cardiovascular complications. However, the association between HbA1c variability and heart failure (HF) risk remains unclear. This meta-analysis aimed to quantify the relationship between HbA1c variability and the risk of incident HF in adults. A systematic search of PubMed, Embase, and Web of Science was conducted to identify relevant studies. Observational studies and post-hoc analyses of clinical trials evaluating the association between visit-to-visit HbA1c variability and incident HF were included. Random-effects models were employed to pool hazard ratios (HRs) with 95% confidence intervals (CIs), accounting for potential heterogeneity. A total of nine studies (n = 342,123) were included in the analysis. Overall, high HbA1c variability was associated with an increased risk of HF (pooled HR = 1.78, 95% CI: 1.39–2.27, p < 0.001; I² = 87%). Sensitivity analyses restricted to patients with type 2 diabetes (HR = 1.73, 95% CI: 1.35–2.22), high-quality studies (HR = 1.82, 95% CI: 1.32–2.50), or studies adjusting for mean HbA1c (HR = 1.68, 95% CI: 1.31–2.16) produced consistent results. Subgroup analyses indicated a stronger association in prospective cohorts (HR = 2.51) compared to retrospective or post-hoc studies (p for subgroup difference < 0.001). Meta-regression analysis revealed no significant modifying effects of age, sex, follow-up duration, or study quality (p all > 0.05). In conclusion, greater visit-to-visit HbA1c variability may be associated with an increased risk of incident HF, underscoring the prognostic importance of maintaining stable long-term glycemic control in patients with type 2 diabetes.
Citations
Downloads
References
Martin SS, Aday AW, Allen NB, Almarzooq ZI, Anderson CAM, Arora P, et al. 2025 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2025;151(8):e41–e660.
Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats AJS. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. 2023;118(17):3272–87.
https://doi.org/10.1093/cvr/cvac013
Bozkurt B. Concerning Trends of Rising Heart Failure Mortality Rates. JACC Heart Fail. 2024;12(5):970–2.
https://doi.org/10.1016/j.jchf.2024.04.001
Triposkiadis F, Xanthopoulos A, Parissis J, Butler J, Farmakis D. Pathogenesis of chronic heart failure: cardiovascular aging, risk factors, comorbidities, and disease modifiers. Heart Fail Rev. 2022;27(1):337–44.
https://doi.org/10.1007/s10741-020-09987-z
Xie S, Xu SC, Deng W, Tang Q. Metabolic landscape in cardiac aging: insights into molecular biology and therapeutic implications. Signal Transduct Target Ther. 2023;8(1):114.
https://doi.org/10.1038/s41392-023-01378-8
Park JJ. Epidemiology, Pathophysiology, Diagnosis and Treatment of Heart Failure in Diabetes. Diabetes Metab J. 2021;45(2):146–57.
https://doi.org/10.4093/dmj.2020.0282
Alfieri V, Myasoedova VA, Vinci MC, Rondinelli M, Songia P, Massaiu I, et al. The Role of Glycemic Variability in Cardiovascular Disorders. Int J Mol Sci. 2021;22(16).
https://doi.org/10.3390/ijms22168393
Caturano A, Rocco M, Tagliaferri G, Piacevole A, Nilo D, Di Lorenzo G, et al. Oxidative Stress and Cardiovascular Complications in Type 2 Diabetes: From Pathophysiology to Lifestyle Modifications. Antioxidants (Basel). 2025;14(1).
https://doi.org/10.3390/antiox14010072
Parrinello CM, Selvin E. Beyond HbA1c and glucose: the role of nontraditional glycemic markers in diabetes diagnosis, prognosis, and management. Curr Diab Rep. 2014;14(11):548.
https://doi.org/10.1007/s11892-014-0548-3
Sakamoto M. Type 2 Diabetes and Glycemic Variability: Various Parameters in Clinical Practice. J Clin Med Res. 2018;10(10):737–42.
https://doi.org/10.14740/jocmr3556w
Ceriello A, Monnier L, Owens D. Glycaemic variability in diabetes: clinical and therapeutic implications. Lancet Diabetes Endocrinol. 2019;7(3):221–30.
https://doi.org/10.1016/S2213-8587(18)30136-0
Umpierrez GE, B PK. Glycemic Variability: How to Measure and Its Clinical Implication for Type 2 Diabetes. Am J Med Sci. 2018;356(6):518–27.
https://doi.org/10.1016/j.amjms.2018.09.010
Li F, Zhang L, Shen Y, Liu HH, Zhang ZY, Hu G, et al. Higher glucose fluctuation is associated with a higher risk of cardiovascular disease: Insights from pooled results among patients with diabetes. J Diabetes. 2023;15(5):368–81.
https://doi.org/10.1111/1753-0407.13386
Qu F, Shi Q, Wang Y, Shen Y, Zhou K, Pearson ER, et al. Visit-to-visit glycated hemoglobin A1c variability in adults with type 2 diabetes: a systematic review and meta-analysis. Chin Med J (Engl). 2022;135(19):2294–300.
https://doi.org/10.1097/CM9.0000000000002073
Tabesh M, Sacre JW, Mehta K, Chen L, Sajjadi SF, Magliano DJ, et al. The association of glycaemic risk factors and diabetes duration with risk of heart failure in people with type 2 diabetes: A systematic review and meta-analysis. Diabetes Obes Metab. 2024;26(12):5690–700.
https://doi.org/10.1111/dom.15938
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
https://doi.org/10.1136/bmj.n71
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.2. The Cochrane Collaboration. 2021.
https://www.training.cochrane.org/handbook
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2010.
http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
https://doi.org/10.1002/sim.1186
Marušić MF, Fidahić M, Cepeha CM, Farcaș LG, Tseke A, Puljak L. Methodological tools and sensitivity analysis for assessing quality or risk of bias used in systematic reviews published in the high-impact anesthesiology journals. BMC Medical Research Methodology. 2020;20(1):121.
https://doi.org/10.1186/s12874-020-00966-4
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
https://doi.org/10.1136/bmj.315.7109.629
Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
https://doi.org/10.1111/j.0006-341X.2000.00455.x
Guo J, Fan YQ, Zhang JF, Wang CQ. Association of hemoglobin A1c variability and the incidence of heart failure with preserved ejection fraction in patients with type 2 diabetes mellitus and arterial hypertension. Hellenic J Cardiol. 2018;59(2):91–7.
https://doi.org/10.1016/j.hjc.2017.08.001
Kaze AD, Santhanam P, Erqou S, Ahima RS, Echouffo-Tcheugui JB. Long-term variability of glycemic markers and risk of all-cause mortality in type 2 diabetes: the Look AHEAD study. BMJ Open Diabetes Res Care. 2020;8(2).
https://doi.org/10.1136/bmjdrc-2020-001753
Li S, Nemeth I, Donnelly L, Hapca S, Zhou K, Pearson ER. Visit-to-Visit HbA(1c) Variability Is Associated With Cardiovascular Disease and Microvascular Complications in Patients With Newly Diagnosed Type 2 Diabetes. Diabetes Care. 2020;43(2):426–32.
https://doi.org/10.2337/dc19-0823
Segar MW, Patel KV, Vaduganathan M, Caughey MC, Butler J, Fonarow GC, et al. Association of Long-term Change and Variability in Glycemia With Risk of Incident Heart Failure Among Patients With Type 2 Diabetes: A Secondary Analysis of the ACCORD Trial. Diabetes Care. 2020;43(8):1920–8.
https://doi.org/10.2337/dc19-2541
Wan EYF, Yu EYT, Chin WY, Ng FTY, Chia SMC, Wong ICK, et al. Age-specific associations of glycated haemoglobin variability with cardiovascular disease and mortality in patients with type 2 diabetes mellitus: A 10-year cohort study. Diabetes Obes Metab. 2020;22(8):1316–27.
https://doi.org/10.1111/dom.14034
Lin YT, Huang WL, Wu HP, Chang MP, Chen CC. Association of Mean and Variability of HbA1c with Heart Failure in Patients with Type 2 Diabetes. J Clin Med. 2021;10(7).
https://doi.org/10.3390/jcm10071401
Ceriello A, Lucisano G, Prattichizzo F, La Grotta R, Franzen S, Svensson AM, et al. HbA1c variability predicts cardiovascular complications in type 2 diabetes regardless of being at glycemic target. Cardiovasc Diabetol. 2022;21(1):13.
https://doi.org/10.1186/s12933-022-01445-4
Manosroi W, Phimphilai M, Waisayanand N, Buranapin S, Deerochanawong C, Gunaparn S, et al. Glycated hemoglobin variability and the risk of cardiovascular events in patients with prediabetes and type 2 diabetes mellitus: A post-hoc analysis of a prospective and multicenter study. J Diabetes Investig. 2023;14(12):1391–400.
https://doi.org/10.1111/jdi.14073
Hsiao FC, Lin CP, Hsu TJ, Tung YC, Chan YH, Chen SW, et al. Glycohemoglobin Variations and Long-term Risk of Incident Heart Failure in Patients With Type 2 Diabetes. Mayo Clin Proc. 2025;100(8):1332–44.
https://doi.org/10.1016/j.mayocp.2024.12.022
Roy B. Pathophysiological Mechanisms of Diabetes-Induced Macrovascular and Microvascular Complications: The Role of Oxidative Stress. Med Sci (Basel). 2025;13(3).
https://doi.org/10.3390/medsci13030087
Liu TS, Pei YH, Peng YP, Chen J, Jiang SS, Gong JB. Oscillating high glucose enhances oxidative stress and apoptosis in human coronary artery endothelial cells. J Endocrinol Invest. 2014;37(7):645–51.
https://doi.org/10.1007/s40618-014-0086-5
Murata M, Adachi H, Oshima S, Kurabayashi M. Glucose fluctuation and the resultant endothelial injury are correlated with pancreatic β cell dysfunction in patients with coronary artery disease. Diabetes Res Clin Pract. 2017;131:107–15.
https://doi.org/10.1016/j.diabres.2017.07.007
Watanabe M, Kawai Y, Kitayama M, Akao H, Motoyama A, Wakasa M, et al. Diurnal glycemic fluctuation is associated with severity of coronary artery disease in prediabetic patients: Possible role of nitrotyrosine and glyceraldehyde-derived advanced glycation end products. J Cardiol. 2017;69(4):625–31.
https://doi.org/10.1016/j.jjcc.2016.07.001
Mordel P, Fontaine F, Dupas Q, Joubert M, Allouche S. Glucose fluctuation promotes mitochondrial dysfunctions in the cardiomyocyte cell line HL-1. PLoS One. 2023;18(9):e0289475.
https://doi.org/10.1371/journal.pone.0289475
Zhang L, Liu HH, Yang F, Zhang ZY, Zhao XX, Qian LL, et al. Glucose fluctuations aggravate myocardial fibrosis via activating the CaMKII/Stat3 signaling in type 2 diabetes. Diabetol Metab Syndr. 2023;15(1):217.
https://doi.org/10.1186/s13098-023-01197-5
Brahma MK, Pepin ME, Wende AR. My Sweetheart Is Broken: Role of Glucose in Diabetic Cardiomyopathy. Diabetes Metab J. 2017;41(1):1–9.
https://doi.org/10.4093/dmj.2017.41.1.1
Vural Keskinler M, Takir M, Caklili OT, Oguz A. The Frequency and Determinants of HbA1c Variability in Type 2 Diabetic Patients. Metab Syndr Relat Disord. 2021;19(7):372–7.
https://doi.org/10.1089/met.2020.0131
Wu TE, Su YW, Chen HS. Mean HbA1c and HbA1c variability are associated with differing diabetes-related complications in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2022;192:110069.
https://doi.org/10.1016/j.diabres.2022.110069
Aroda VR, Eckel RH. Reconsidering the role of glycaemic control in cardiovascular disease risk in type 2 diabetes: A 21st century assessment. Diabetes Obes Metab. 2022;24(12):2297–308.
https://doi.org/10.1111/dom.14830
Huang Y, Heng C, Wei J, Jing X, Wang X, Zhao G, et al. Influencing factors of glycemic variability in hospitalized type 2 diabetes patients with insulin therapy: A Strobe-compliant article. Medicine (Baltimore). 2017;96(36):e8021.
https://doi.org/10.1097/MD.0000000000008021
Zhou Z, Sun B, Huang S, Zhu C, Bian M. Glycemic variability: adverse clinical outcomes and how to improve it? Cardiovasc Diabetol. 2020;19(1):102.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Guo Mujiafu Qiao Longbatu, La Xinamujila, Bao Burie

This work is licensed under a Creative Commons Attribution 4.0 International License.









