Tubeless uniportal VATS in thoracic surgery – Indications, ERAS pathways, and outcomes: A review
DOI:
https://doi.org/10.17305/bb.2026.13644Keywords:
Tubeless thoracic surgery, uniportal video-assisted thoracoscopic surgery, minimally invasive thoracic surgery, non-intubated anesthesia, chest drain-free surgery, enhanced recovery after surgery, ERASAbstract
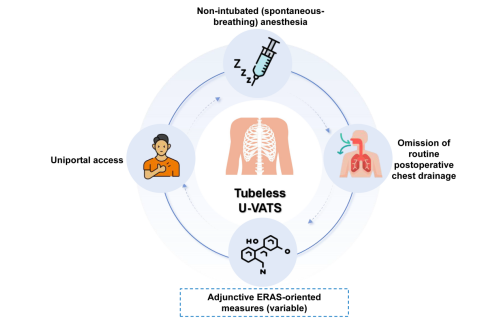
Tubeless uniportal video-assisted thoracoscopic surgery (VATS) is an innovative approach characterized by the use of non-intubated (spontaneous-breathing) anesthesia, the omission of routine postoperative chest drainage, and single-port access. This technique has gained traction in recent years for a variety of thoracic procedures. While practices reported in the literature may differ, this review primarily examines the combined non-intubated and drainless approach. This narrative review provides a comprehensive overview and critical analysis of its current clinical applications, including sympathectomy, pulmonary wedge resection, spontaneous pneumothorax, thymectomy, and early-stage lung cancer. It also addresses essential aspects of perioperative management and procedural indications within enhanced recovery-oriented pathways. A systematic literature search of PubMed, Embase, and Web of Science was conducted to identify pertinent studies published between January 2010 and April 2025. Current clinical reports indicate potential benefits such as reduced postoperative pain, shorter hospital stays, and accelerated recovery. However, the existing evidence largely stems from small, observational studies with varied methodologies, necessitating cautious interpretation. The broader implementation of this technique in more complex procedures depends on the establishment of standardized clinical pathways, the refinement of multidisciplinary perioperative strategies, and validation through multicenter prospective studies. Tubeless uniportal VATS shows promise as a significant advancement in function-preserving and recovery-oriented thoracic surgery.
Citations
Downloads
References
Geldenhuys A. Thoracic damage control surgery. Current Trauma Reports. 2018;4:177–82.
https://doi.org/10.1007/s40719-018-0137-z
Yan Y, Huang Q, Han H, Zhang Y, Chen H. Uniportal versus multiportal video-assisted thoracoscopic anatomical resection for NSCLC: a meta-analysis. J Cardiothorac Surg. 2020;15(1):238.
https://doi.org/10.1186/s13019-020-01280-2
Shen C, Che G. No drains in thoracic surgery with ERAS program. J Cardiothorac Surg. 2020;15(1):112.
https://doi.org/10.1186/s13019-020-01164-5
Liu CY, Hsu PK, Chien HC, Hsieh CC, Ting CK, Tsou MY. Tubeless single-port thoracoscopic sublobar resection: indication and safety. J Thorac Dis. 2018;10(6):3729–37.
https://doi.org/10.21037/jtd.2018.05.119
Koh LY, Hwang NC. Anesthesia for nonintubated video-assisted thoracoscopic surgery. J Cardiothorac Vasc Anesth. 2023;37(7):1275–83.
https://doi.org/10.1053/j.jvca.2023.02.048
Liu J, Liang H, Cui F, Liu H, Zhu C, Liang W, et al. Spontaneous versus mechanical ventilation during video-assisted thoracoscopic surgery for spontaneous pneumothorax: a randomized trial. J Thorac Cardiovasc Surg. 2022;163(5):1702–14.e7.
Huang K, Zhang Z, Hu T, Qiao L. Advances in the use of non-intubated spontaneous-ventilation video-assisted thoracoscopic surgery. Front Surg. 2025;12:1584017.
https://doi.org/10.3389/fsurg.2025.1584017
Hung MH, Hsu HH, Cheng YJ, Chen JS. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis. 2014;6(1):2–9.
Cui F, Liu J, Li S, Yin W, Xin X, Shao W, et al. Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively. J Thorac Dis. 2016;8(8):2226–32.
https://doi.org/10.21037/jtd.2016.08.02
He J, Liu J, Zhu C, Dai T, Cai K, Zhang Z, et al. Expert consensus on tubeless video-assisted thoracoscopic surgery (Guangzhou). J Thorac Dis. 2019;11(10):4101–8.
https://doi.org/10.21037/jtd.2019.10.04
Janik M, Juhos P, Lucenic M, Tarabova K. Non-intubated thoracoscopic surgery – pros and cons. Front Surg. 2021;8:801718.
https://doi.org/10.3389/fsurg.2021.801718
Umari M, Falini S, Segat M, Zuliani M, Crisman M, Comuzzi L, et al. Anesthesia and fast-track in video-assisted thoracic surgery (VATS): from evidence to practice. J Thorac Dis. 2018;10(Suppl 4):S542–S54.
https://doi.org/10.21037/jtd.2017.12.83
Khoury AL, Kolarczyk LM, Strassle PD, Feltner C, Hance LM, Teeter EG, et al. Thoracic enhanced recovery after surgery: single academic center observations after implementation. Ann Thorac Surg. 2021;111(3):1036–43.
https://doi.org/10.1016/j.athoracsur.2020.06.021
Zhao Y, Shan L, Zhang W, Li P, Li N, Zhang H, et al. Minimally invasive lung surgery with an intraoperative completely or partially tubeless protocol: randomized clinical trial. BJS Open. 2024;9(1):zrae132.
https://doi.org/10.1093/bjsopen/zrae132
Huang Y, Bo Y, Li Y, Zhao Y, Li X, Chen D, et al. The impact of tubeless anesthesia versus intubated anesthesia on cerebral oxygen saturation and postoperative cognitive function in patients undergoing video-assisted thoracoscopic surgery: a randomized trial. J Thorac Dis. 2022;14(10):4012–30.
https://doi.org/10.21037/jtd-22-1165
Szabo Z, Fabo C, Oszlanyi A, Hawchar F, Geczi T, Lantos J, et al. Anesthetic (r)evolution from the conventional concept to the minimally invasive techniques in thoracic surgery: narrative review. J Thorac Dis. 2022;14(8):3045–60.
https://doi.org/10.21037/jtd-22-80
Pompeo E. From awake to minimalist spontaneous ventilation thoracoscopic lung surgery: an ongoing journey. J Clin Med. 2025;14(7):2475.
https://doi.org/10.3390/jcm14072475
Batchelor TJP. Enhanced recovery after surgery and chest tube management. J Thorac Dis. 2023;15(2):901–8.
https://doi.org/10.21037/jtd-22-1373
Tsai CS, Tung HH, Fang CJ, Chen CT. Effectiveness of non-pharmacological interventions for pain reduction following chest tube removal: a systematic review and network meta-analysis. Intensive Crit Care Nurs. 2025;87:103909.
https://doi.org/10.1016/j.iccn.2024.103909
Hung WT, Cheng YJ, Chen JS. Video-assisted thoracoscopic surgery lobectomy for lung cancer in nonintubated anesthesia. Thorac Surg Clin. 2020;30(1):73–82.
https://doi.org/10.1016/j.thorsurg.2019.09.002
Fu Z, Wang L, Hu W, Zhou Y, Zhou Q. Comparison of the efficacy of subxiphoid and intercostal uniportal video-assisted thoracoscopic surgery in patients with early-stage non-small cell lung cancer. Pak J Med Sci. 2025;41(2):359–65.
https://doi.org/10.12669/pjms.41.2.11096
Alanwar M, Elsharawy M, Brik A, Ahmady I, Shemais DS. Safety and perioperative outcomes of uniportal versus multiportal video-assisted thoracoscopic surgery. J Minim Access Surg. 2024;20(3):294–300.
https://doi.org/10.4103/jmas.jmas_84_23
Elsayed HH, Moharram AA. Tailored anaesthesia for thoracoscopic surgery promoting enhanced recovery: the state of the art. Anaesth Crit Care Pain Med. 2021;40(2):100846.
https://doi.org/10.1016/j.accpm.2021.100846
Wang LF, Qi F, Feng HX, Shi YH, Li Y, Zheng MT, et al. Risk and benefit analysis of single-shot nerve block for postoperative analgesia for uniportal video-assisted thoracic surgery (uVATS): a randomized controlled trial. BMC Anesthesiol. 2025;25(1):68.
https://doi.org/10.1186/s12871-025-02955-w
Galvez C, Bolufer S, Galvez E, Navarro-Martinez J, Galiana-Ivars M, Sesma J, et al. Anatomic segmentectomy in nonintubated video-assisted thoracoscopic surgery. Thorac Surg Clin. 2020;30(1):61–72.
https://doi.org/10.1016/j.thorsurg.2019.09.003
Tacconi F, Pompeo E. Non-intubated video-assisted thoracic surgery: where does evidence stand? J Thorac Dis. 2016;8(Suppl 4):S364–75.
https://doi.org/10.21037/jtd.2016.04.39
Jo Y, Park S, Oh C, Pak Y, Jeong K, Yun S, et al. Regional analgesia techniques for video-assisted thoracic surgery: a frequentist network meta-analysis. Korean J Anesthesiol. 2022;75(3):231–44.
https://doi.org/10.4097/kja.21330
Fabo C, Oszlanyi A, Lantos J, Rarosi F, Horvath T, Barta Z, et al. Non-intubated thoracoscopic surgery – tips and tricks from anesthesiological aspects: a mini review. Front Surg. 2021;8:818456.
https://doi.org/10.3389/fsurg.2021.818456
Chen KC, Cheng YJ, Hung MH, Tseng YD, Chen JS. Nonintubated thoracoscopic lung resection: a 3-year experience with 285 cases in a single institution. J Thorac Dis. 2012;4(4):347–51.
Gonzalez-Rivas D, Bonome C, Fieira E, Aymerich H, Fernandez R, Delgado M, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg. 2016;49(3):721–31.
https://doi.org/10.1093/ejcts/ezv136
Shao GQ, Pang DZ, Zhang JT, Wang HX, Liuru TY, Liu ZH, et al. Spontaneous ventilation anesthesia combined with uniportal and tubeless thoracoscopic sympathectomy in selected patients with primary palmar hyperhidrosis. J Cardiothorac Surg. 2022;17(1):177.
https://doi.org/10.1186/s13019-022-01917-4
Sang HW, Li GL, Xiong P, Zhu MC, Zhu M. Optimal targeting of sympathetic chain levels for treatment of palmar hyperhidrosis: an updated systematic review. Surg Endosc. 2017;31(11):4357–69.
https://doi.org/10.1007/s00464-017-5508-y
Chen JF, Lin JB, Tu YR, Lin M, Li X, Lai FC, et al. Nonintubated transareolar single-port thoracic sympathicotomy with a needle scope in a series of 85 male patients. Surg Endosc. 2016;30(8):3447–53.
https://doi.org/10.1007/s00464-015-4628-5
Cao J, Gao X, Zhang X, Li J, Zhang J. Feasibility of laryngeal mask anesthesia combined with nerve block in adult patients undergoing internal fixation of rib fractures: a prospective observational study. BMC Anesthesiol. 2020;20(1):170.
https://doi.org/10.1186/s12871-020-01082-y
Magouliotis DE, Karamolegkou AP, Zotos PA, Minervini F, Cioffi U, Scarci M. Is less more? A meta-analysis of non-intubated versus intubated VATS for anatomic resections in non-small cell lung cancer. J Clin Med. 2025;14(19):6731.
https://doi.org/10.3390/jcm14196731
Majeed ZS, Baram A, Izac AY. Quality of life and patient satisfaction after single-port endoscopic thoracic sympathectomy for primary focal hyperhidrosis: a follow-up of 250 patients. International Journal of Surgery Open. 2024;62(4):373–8.
https://doi.org/10.1097/IO9.0000000000000097
Igai H, Matsuura N, Numajiri K, Ohsawa F, Kamiyoshihara M. Feasibility of tubeless thoracoscopic bullectomy in primary spontaneous pneumothorax patients. Gen Thorac Cardiovasc Surg. 2023;71(2):138–44.
https://doi.org/10.1007/s11748-022-01869-5
Li X, Wang X, Zhang H, Cheng H, Cao Q. Unilateral single-port thoracoscopic surgery for bilateral pneumothorax or pulmonary bullae. J Cardiothorac Surg. 2019;14(1):71.
https://doi.org/10.1186/s13019-019-0894-y
Chen PH, Hung WT, Chen JS. Nonintubated video-assisted thoracic surgery for the management of primary and secondary spontaneous pneumothorax. Thorac Surg Clin. 2020;30(1):15–24.
https://doi.org/10.1016/j.thorsurg.2019.08.001
Mineo TC, Ambrogi V, Sellitri F. Non-intubated video-assisted thoracic surgery from multi to uniport approaches: single-centre experience. Eur Med J Respir. 2016;4:104–12.
https://doi.org/10.33590/emjrespir/10312090
Cui W, Huang D, Liang H, Peng G, Liu M, Li R, et al. Tubeless video-assisted thoracoscopic surgery in mediastinal tumor resection. Gland Surg. 2021;10(4):1387–96.
https://doi.org/10.21037/gs-20-682
Németh T. Pathophysiological background and perioperative outcome of thymus removal with spontaneous ventilation by intubation. Moving Forward With Minimal Invasiveness. Szeged University (Hungary); 2023.
Rosboch GL, Lyberis P, Ceraolo E, Balzani E, Cedrone M, Piccioni F, et al. The anesthesiologist's perspective regarding non-intubated thoracic surgery: a scoping review. Front Surg. 2022;9:868287.
https://doi.org/10.3389/fsurg.2022.868287
Liu Z, Zhang L, Tang W, Yang R. Non-intubated uniportal subxiphoid thoracoscopic extended thymectomy for thymoma associated with myasthenia gravis. World J Surg Oncol. 2021;19(1):342.
https://doi.org/10.1186/s12957-021-02430-z
Moon MH. Beyond the limits: journey to feasible and safe uniportal VATS surgery for lung cancer. J Thorac Dis. 2023;15(2):246–9.
https://doi.org/10.21037/jtd-22-1877
Yang SM, Hsu HH, Chen JS. Recent advances in surgical management of early lung cancer. J Formos Med Assoc. 2017;116(12):917–23.
https://doi.org/10.1016/j.jfma.2017.07.009
Kreso A, Mathisen DJ. Management of air leaks and residual spaces following lung resection. Thorac Surg Clin. 2021;31(3):265–71.
https://doi.org/10.1016/j.thorsurg.2021.04.005
Messina G, Natale G, Bove M, Opromolla G, Di Filippo V, Martone M, et al. Intraoperative ventilatory leak: real-time guidance for management of air leak in lung cancer patients undergoing VATS lobectomy. Thorac Cancer. 2023;14(18):1782–8.
https://doi.org/10.1111/1759-7714.14925
He J, Liang H, Wang W, Akopov A, Aiolfi A, Ang KL, et al. Tubeless video-assisted thoracic surgery for pulmonary ground-glass nodules: expert consensus and protocol (Guangzhou). Transl Lung Cancer Res. 2021;10(8):3503–19.
https://doi.org/10.21037/tlcr-21-663
Scarci M, Gkikas A, Patrini D, Minervini F, Cerfolio RJ. Editorial: early chest drain removal following lung resection. Front Surg. 2023;10:1185334.
https://doi.org/10.3389/fsurg.2023.1185334
Yu J, Tantraworasin A, Laohathai S. Non-intubated versus intubated video-assisted thoracoscopic lobectomy for lung cancer patients. Asian J Surg. 2024;47(1):402–6.
https://doi.org/10.1016/j.asjsur.2023.09.038
Watanabe T, Tanahashi M, Chiba M, Hashimoto K, Sakakura N, Okazaki M, et al. Postoperative pain reduction and clinical value of uniportal video-assisted thoracic surgery: a secondary analysis of the J-RATSIG 01 study. Clin Lung Cancer. 2025.
https://doi.org/10.5090/jcs.2025S1.25S-0007
Holbek BL, Hansen HJ, Kehlet H, Petersen RH. Thoracoscopic pulmonary wedge resection without post-operative chest drain: an observational study. Gen Thorac Cardiovasc Surg. 2016;64(10):612–7.
https://doi.org/10.1007/s11748-016-0692-6
Wang R, Wang Q, Jiang S, Chen C, Zheng J, Liu H, et al. Spontaneous ventilation video-assisted thoracoscopic surgery for non-small-cell lung cancer patients with poor lung function: short- and long-term outcomes. Front Surg. 2022;9:800082.
https://doi.org/10.3389/fsurg.2022.800082
Anile M, Vannucci J, Ferrante F, Bruno K, De Paolo D, Bassi M, et al. Non-intubated thoracic surgery: standpoints and perspectives. Front Surg. 2022;9:937633.
https://doi.org/10.3389/fsurg.2022.937633
Cherchi R, Ferrari PA, Guerrera F, Grimaldi G, Pinna-Susnik M, Murenu A, et al. Lung biopsy with a non-intubated VATS approach in an obese population: indications and results. Front Surg. 2022;9:829976.
https://doi.org/10.3389/fsurg.2022.829976
Grott M, Eichhorn M, Eichhorn F, Schmidt W, Kreuter M, Winter H. Thoracic surgery in the non-intubated spontaneously breathing patient. Respir Res. 2022;23(1):379.
https://doi.org/10.1186/s12931-022-02250-z
Furak J, Szabo Z, Tanczos T, Paszt A, Rieth A, Nemeth T, et al. Conversion method to manage surgical difficulties in non-intubated uniportal video-assisted thoracic surgery for major lung resection: simple thoracotomy without intubation. J Thorac Dis. 2020;12(5):2061–9.
https://doi.org/10.21037/jtd-19-3830
Abbaker N, Minervini F, Guttadauro A, Solli P, Cioffi U, Scarci M. The future of artificial intelligence in thoracic surgery for non-small cell lung cancer treatment: a narrative review. Front Oncol. 2024;14:1347464.
https://doi.org/10.3389/fonc.2024.1347464
Poullis M. The transformation of risk modelling in cardiac and thoracic surgery through artificial intelligence. Eur J Cardiothorac Surg. 2024;65(1):ezae013.
https://doi.org/10.1093/ejcts/ezae013
Li S, Jiang L, Ang KL, Chen H, Dong Q, Yang H, et al. New tubeless video-assisted thoracoscopic surgery for small pulmonary nodules. Eur J Cardiothorac Surg. 2017;51(4):689–93.
https://doi.org/10.1093/ejcts/ezw364
Yang SM, Wang ML, Hung MH, Hsu HH, Cheng YJ, Chen JS. Tubeless uniportal thoracoscopic wedge resection for peripheral lung nodules. Ann Thorac Surg. 2017;103(2):462–8.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2026 Bo Zhang, Xian-hua Ye, De-shuang Xiao

This work is licensed under a Creative Commons Attribution 4.0 International License.









