The long-term outcome and risk factors for precursor B cell acute lymphoblastic leukemia without specific fusion genes in Chinese children: experiences from multiple centers
DOI:
https://doi.org/10.17305/bjbms.2021.5879Keywords:
B-cell acute lymphoblastic leukemia, children, fusion genes, treatment response, minimal residual disease, next-generation sequencingAbstract
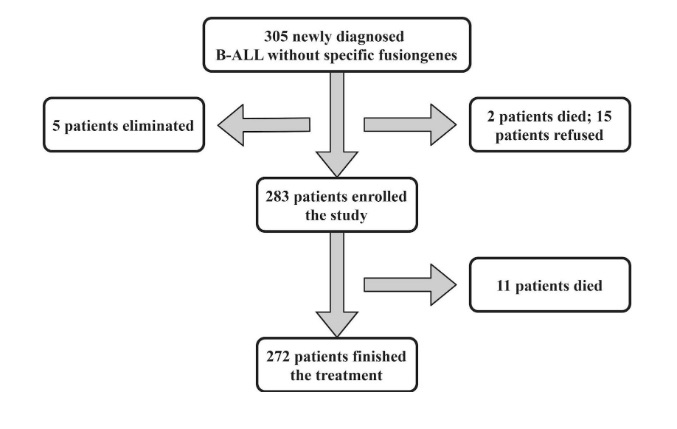
Specific fusion genes play important roles as risk factors for strategic treatment in pediatric B-cell acute lymphoblastic leukemia (B-ALL), and the risk factors in patients without common fusion genes have not been well demonstrated. We collected and analyzed clinical and laboratory findings, treatment responses and outcomes in B-ALL patients without specific fusion genes. Whole-exome sequencing (WES) and/or RNA sequencing (RNAseq) data from bone marrow relapsed patients were also analyzed. 283 patients were enrolled in the study. Traditional elements and treatment responses at different time points (TPs) were evaluated to classify risk groups and adjust the treatment strategy. Treatment-related mortality was found in 11 (3.89%) patients, 49 (17.31%) patients relapsed, and the ten-year prospective event-free survival (pEFS) was 78.2±2.5%. Univariate analysis revealed that significant differences were not found in the pEFS of traditional risk factors, including sex, age, WBC count or chromosome status; good responses of BM smears at TP1 and minimal residual disease (MRD) levels at TP2 and TP3 were strongly associated with prolonged pEFS. Compared with the IR or the HR group, patients in the SR group presented with longer pEFS and a lower relapse rate. Multivariable analysis of outcomes and hazard ratios revealed that a positive MRD level was a key risk factor. WES or RNAseq was performed for BM relapse patients, and adverse and unreported genetic abnormalities were discovered. Favorable outcomes were acquired in the cohort. The study results showed that traditional risk factors and poor prednisone response were overcome by modified chemotherapy, and a positive MRD level was a key risk factor in these patients. NGS is needed to discover more risk-related molecular abnormalities.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2021-07-15
Published 2022-04-01









