Synergistic effect of the rifaximin–berberine combination against Klebsiella pneumoniae: RfaH targeting supported by MD simulation
DOI:
https://doi.org/10.17305/bb.2026.13776Keywords:
Synergistic effect, rifaximin-berberine, anti-termination protein RFAH, MD simulation, antibiotic resistance, K. pnuemoniaeAbstract
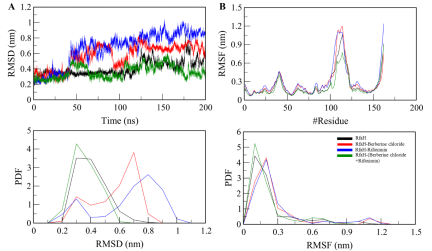
The escalating crisis of antimicrobial resistance (AMR) among Gram-negative pathogens, particularly Klebsiella pneumoniae (KP), necessitates innovative strategies to enhance the efficacy of existing antibiotics. Synergistic drug combinations present a promising approach to improve therapeutic outcomes and delay the emergence of resistance. This study investigates the synergistic interaction between the natural alkaloid berberine chloride and the repurposed antibiotic rifaximin against KP. Integrated in vitro and in silico analyses reveal significant bactericidal synergy between the two agents, mediated through concurrent inhibition of the transcriptional anti-termination factor RfaH, a key regulator of virulence and capsule biosynthesis. Molecular docking and dynamics simulations demonstrate that both compounds cooperatively bind to the RfaH pocket, stabilizing an inactive ternary complex without major structural disruption. Functional assays confirm that the combination effectively suppresses RfaH-dependent capsule production at lower concentrations compared to monotherapy. These findings suggest that RfaH is a viable target for combinatorial inhibition and provide a plausible mechanistic foundation for the berberine–rifaximin synergy. This work supports the rational development of dual-targeting anti-virulence strategies to combat multidrug-resistant KP infections.
Citations
Downloads
References
Effah CY, Sun T, Liu S, Wu Y. Klebsiella pneumoniae: an increasing threat to public health. Annals of clinical microbiology and antimicrobials. 2020;19:1–9.
https://doi.org/10.1186/s12941-019-0343-8
Douradinha B. Should multidrug resistant Klebsiella pneumoniae strains displaying hypervirulent traits be reclassified as either ultravirulent or supervirulent? Microbiol Res. 2023;275:127446.
https://doi.org/10.1016/j.micres.2023.127446
Li L, Li S, Wei X, Lu Z, Qin X, Li M. Infection with carbapenem-resistant hypervirulent Klebsiella pneumoniae: clinical, virulence and molecular epidemiological characteristics. Antimicrobial Resistance & Infection Control. 2023;12(1):124.
https://doi.org/10.1186/s13756-023-01331-y
Sati H, Carrara E, Savoldi A, Hansen P, Garlasco J, Campagnaro E, et al. The WHO bacterial priority pathogens list 2024: a prioritisation study to guide research, development, and public health strategies against antimicrobial resistance. The Lancet infectious diseases. 2025.
https://doi.org/10.1016/S1473-3099(25)00118-5
Gan L, Mao P, Tian Z, Li X, Yu Z, Du B, et al. Higher prevalence of hypervirulent Klebsiella pneumoniae isolates with high-risk multidrug resistance in Asia. Journal of Infection and Public Health. 2025;18(9):102834.
https://doi.org/10.1016/j.jiph.2025.102834
Douradinha B. Exploring the journey: a comprehensive review of vaccine development against Klebsiella pneumoniae. Microbiol Res. 2024;287:127837.
https://doi.org/10.1016/j.micres.2024.127837
Li Y, Kumar S, Zhang L. Mechanisms of antibiotic resistance and developments in therapeutic strategies to combat Klebsiella pneumoniae infection. Infection and Drug Resistance. 2024:1107–19.
https://doi.org/10.2147/IDR.S453025
Saeed MU, Ahmed S, Choudhury A, Hussain A, Alajmi MF, Mohammad T, et al. Discovering novel inhibitors of RfaH from Klebsiella pneumoniae to combat antimicrobial resistance. Archives of Microbiology. 2024;206(12):472.
https://doi.org/10.1007/s00203-024-04192-0
Wu K-M, Li L-H, Yan J-J, Tsao N, Liao T-L, Tsai H-C, et al. Genome sequencing and comparative analysis of Klebsiella pneumoniae NTUH-K2044, a strain causing liver abscess and meningitis. Journal of bacteriology. 2009;191(14):4492–501.
https://doi.org/10.1128/JB.00315-09
Tian D, Liu X, Chen W, Zhou Y, Hu D, Wang W, et al. Prevalence of hypervirulent and carbapenem-resistant Klebsiella pneumoniae under divergent evolutionary patterns. Emerging microbes & infections. 2022;11(1):1936–49.
https://doi.org/10.1080/22221751.2022.2103454
Russo TA, Marr CM. Hypervirulent Klebsiella pneumoniae. Clinical microbiology reviews. 2019;32(3):e00001–19.
https://doi.org/10.1128/CMR.00001-19
Bezerra dos Santos AT, Araújo TFdS, Nascimento da Silva LC, Silva CBd, Oliveira AFMd, Araújo JM, et al. Organic extracts from Indigofera suffruticosa leaves have antimicrobial and synergic actions with erythromycin against Staphylococcus aureus. Frontiers in Microbiology. 2015;6:13.
https://doi.org/10.3389/fmicb.2015.00013
Sasidharan S, Tripathi T, Saudagar P. Critical insight into plausible acquired tocopherol pathway in neglected human trypanosomatids. ACS omega. 2021;6(47):31396–403.
https://doi.org/10.1021/acsomega.1c05046
Saifi S, Ashraf A, Hasan GM, Shamsi A, Hassan MI. Insights into the preventive actions of natural compounds against Klebsiella pneumoniae infections and drug resistance. Fitoterapia. 2024;173:105811.
https://doi.org/10.1016/j.fitote.2023.105811
Yan D, Jin C, Xiao X-H, Dong X-P. Antimicrobial properties of berberines alkaloids in Coptis chinensis Franch by microcalorimetry. Journal of biochemical and biophysical methods. 2008;70(6):845–9.
https://doi.org/10.1016/j.jbbm.2007.07.009
Xia S, Ma L, Wang G, Yang J, Zhang M, Wang X, et al. In vitro antimicrobial activity and the mechanism of berberine against methicillin-resistant Staphylococcus aureus isolated from bloodstream infection patients. Infection and Drug Resistance. 2022;15:1933–44.
https://doi.org/10.2147/IDR.S357077
Noghabi SA, Bagherzade G, Beyzaei H. Comparative study of antioxidant and antimicrobial activity of berberine-derived Schiff bases, nitro-berberine and amino-berberine. Heliyon. 2023;9(12):e22783.
https://doi.org/10.1016/j.heliyon.2023.e22783
Ashraf A, Choudhary A, Khan MA, Noor S, Islam A, Hassan MI. Repurposing rifaximin against Klebsiella pneumoniae via targeting of transcription anti-termination protein RfaH for novel antimicrobial development. 2024.
https://doi.org/10.21203/rs.3.rs-4724428/v1
Ali S, Alam M, Hasan GM, Hassan MI. Potential therapeutic targets of Klebsiella pneumoniae: a multi-omics review perspective. Brief Funct Genomics. 2022;21(2):63–77.
https://doi.org/10.1093/bfgp/elab038
Anwar S, Khan S, Shamsi A, Anjum F, Shafie A, Islam A, et al. Structure-based investigation of MARK4 inhibitory potential of naringenin for therapeutic management of cancer and neurodegenerative diseases. Journal of cellular biochemistry. 2021;122(10):1445–59.
https://doi.org/10.1002/jcb.30022
Dahiya R, Mohammad T, Roy S, Anwar S, Gupta P, Haque A, et al. Investigation of inhibitory potential of quercetin to the pyruvate dehydrogenase kinase 3: towards implications in anticancer therapy. International journal of biological macromolecules. 2019;136:1076–85.
https://doi.org/10.1016/j.ijbiomac.2019.06.158
Gulzar M, Ali S, Khan FI, Khan P, Taneja P, Hassan MI. Binding mechanism of caffeic acid and simvastatin to the integrin linked kinase for therapeutic implications: a comparative docking and MD simulation studies. Journal of Biomolecular Structure and Dynamics. 2019;37(16):4327–37.
https://doi.org/10.1080/07391102.2018.1546621
Kowalska-Krochmal B, Dudek-Wicher R. The minimum inhibitory concentration of antibiotics: methods, interpretation, clinical relevance. Pathogens. 2021;10:165.
https://doi.org/10.3390/pathogens10020165
Rodríguez-Melcón C, Alonso-Calleja C, García-Fernández C, Carballo J, Capita R. Minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) for twelve antimicrobials (biocides and antibiotics) in eight strains of Listeria monocytogenes. Biology. 2021;11(1):46.
https://doi.org/10.3390/biology11010046
Petersen PJ, Labthavikul P, Jones CH, Bradford PA. In vitro antibacterial activities of tigecycline in combination with other antimicrobial agents determined by chequerboard and time-kill kinetic analysis. Journal of Antimicrobial Chemotherapy. 2006;57(3):573–6.
https://doi.org/10.1093/jac/dki477
Blumenkrantz N, Asboe-Hansen G. New method for quantitative determination of uronic acids. Analytical biochemistry. 1973;54(2):484–9.
https://doi.org/10.1016/0003-2697(73)90377-1
Lin T-L, Yang F-L, Yang A-S, Peng H-P, Li T-L, Tsai M-D, et al. Amino acid substitutions of MagA in Klebsiella pneumoniae affect the biosynthesis of the capsular polysaccharide. PLoS One. 2012;7(10):e46783.
https://doi.org/10.1371/journal.pone.0046783
Svetlov D, Shi D, Twentyman J, Nedialkov Y, Rosen DA, Abagyan R, et al. In silico discovery of small molecules that inhibit RfaH recruitment to RNA polymerase. Molecular microbiology. 2018;110(1):128–42.
https://doi.org/10.1111/mmi.14093
Mohammad T, Mathur Y, Hassan MI. InstaDock: a single-click graphical user interface for molecular docking-based virtual high-throughput screening. Briefings in Bioinformatics. 2021;22(4):bbaa279.
https://doi.org/10.1093/bib/bbaa279
DeLano WL. Pymol: an open-source molecular graphics tool. CCP4 Newsl protein crystallogr. 2002;40(1):82–92.
Hassan MI, Anjum D, Mohammad T, Alam M, Khan MS, Shahwan M, et al. Integrated virtual screening and MD simulation study to discover potential inhibitors of Lyn-kinase: targeting cancer therapy. J Biomol Struct Dyn. 2022:1–11.
https://doi.org/10.1080/07391102.2022.2154849
Jairajpuri DS, Mohammad T, Adhikari K, Gupta P, Hasan GM, Alajmi MF, et al. Identification of sphingosine kinase-1 inhibitors from bioactive natural products targeting cancer therapy. ACS Omega. 2020;5(24):14720–9.
https://doi.org/10.1021/acsomega.0c01511
Van Der Spoel D, Lindahl E, Hess B, Groenhof G, Mark AE, Berendsen HJ. GROMACS: fast, flexible, and free. Journal of computational chemistry. 2005;26(16):1701–18.
https://doi.org/10.1002/jcc.20291
Huang J, MacKerell Jr AD. CHARMM36 all-atom additive protein force field: validation based on comparison to NMR data. Journal of computational chemistry. 2013;34(25):2135–45.
https://doi.org/10.1002/jcc.23354
Cai Q, Yang M, Liu D, Chen J, Shu D, Xia J, et al. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering. 2020;6(10):1192–8.
https://doi.org/10.1016/j.eng.2020.03.007
Bansal KK, Goyal R, Sharma A, Sharma PC, Goyal RK. Repurposing of drugs for the treatment of microbial diseases. Drug Repurposing for Emerging Infectious Diseases and Cancer. 2023:347–94.
https://doi.org/10.1007/978-981-19-5399-6_16
Kang JY, Mooney RA, Nedialkov Y, Saba J, Mishanina TV, Artsimovitch I, et al. Structural basis for transcript elongation control by NusG family universal regulators. Cell. 2018;173(7):1650–62.e14.
https://doi.org/10.1016/j.cell.2018.05.017
Galaz-Davison P, Román EA, Ramírez-Sarmiento CA. The N-terminal domain of RfaH plays an active role in protein fold-switching. PLoS computational biology. 2021;17(9):e1008882.
https://doi.org/10.1371/journal.pcbi.1008882
Bulusu G, Desiraju GR. Strong and weak hydrogen bonds in protein-ligand recognition. Journal of the Indian Institute of Science. 2020;100(1):31–41.
https://doi.org/10.1007/s41745-019-00141-9
de Brevern AG. Impact of protein dynamics on secondary structure prediction. Biochimie. 2020;179:14–22.
https://doi.org/10.1016/j.biochi.2020.09.006
Moradi S, Nowroozi A, Nezhad MA, Jalali P, Khosravi R, Shahlaei M. A review on description dynamics and conformational changes of proteins using combination of principal component analysis and molecular dynamics simulation. Computers in Biology and Medicine. 2024;183:109245.
https://doi.org/10.1016/j.compbiomed.2024.109245
Larsson D, Gaze W, Laxminarayan R, Topp E. AMR, One Health and the environment. Nature Microbiology. 2023;8(5):754–5.
https://doi.org/10.1038/s41564-023-01351-9
Padhi AK, Tripathi T. A comprehensive protein design protocol to identify resistance mutations and signatures of adaptation in pathogens. Briefings in Functional Genomics. 2023;22(2):195–203.
https://doi.org/10.1093/bfgp/elac020
Shukla R, Shukla H, Tripathi T. Structural and energetic understanding of novel natural inhibitors of Mycobacterium tuberculosis malate synthase. Journal of Cellular Biochemistry. 2019;120(2):2469–82.
https://doi.org/10.1002/jcb.27538
Yang M, Dong M, Wu Q-Y, Yao S, Pu G, Ma Y-Y, et al. Three new isoquinoline alkaloids from the fermentation of Aspergillus sp. 0338 and their anti-MRSA activities. Natural Product Research. 2025;39(1):103–9.
https://doi.org/10.1080/14786419.2023.2254455
Ju J, Xie Y, Yu H, Guo Y, Cheng Y, Qian H, et al. Synergistic interactions of plant essential oils with antimicrobial agents: a new antimicrobial therapy. Critical Reviews in Food Science and Nutrition. 2022;62(7):1740–51.
https://doi.org/10.1080/10408398.2020.1846494
Xu L, Li J, Wu W, Wu X, Ren J. Klebsiella pneumoniae capsular polysaccharide: mechanism in regulation of synthesis, virulence, and pathogenicity. Virulence. 2024;15(1):2439509.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2026 Anam Ashraf, Mohammad Ali Khan, Arunabh Choudhury, Swati Kumari, Bader S. Alotaibi, Saba Noor, Mohd Adnan, Md. Imtaiyaz Hassan

This work is licensed under a Creative Commons Attribution 4.0 International License.









